Medicaid In New York State
- COVID-19 News and Updates:
- COVID Information for Medicaid Consumers:
- Medicaid Coverage through Your Local Department of Social Services during the Coronavirus Emergency –
- Medicaid Telehealth Services During the Coronavirus Emergency –
- IRS Form 1095-B Update:
- The 1095-B form for Tax Year 2020 is no longer being mailed automatically.If you need a copy of your 1095-B for Tax Year 2020, you can request it:
- By e-mail – or
Can An Uninsured Woman Enroll In A Public Health Insurance Plan Upon Becoming Pregnant
Yes, women who meet the eligibility criteria for Medicaid or Childrens Health Insurance Program can enroll in one of these public programs at any point during pregnancy:
Full-Scope Medicaid
A pregnant woman is eligible for full-scope Medicaid coverage at any point during pregnancy if eligible under state requirements. Eligibility factors include household size, income, residency in the state of application, and immigration status. An uninsured woman who is already pregnant at the time of application is not eligible for enrollment in expansion Medicaid.
Pregnancy-Related Medicaid
If household income exceeds the income limits for full-scope Medicaid coverage, but is at or below the states income cutoff for pregnancy-related Medicaid, a woman is entitled to Medicaid under the coverage category for pregnancy-related services and conditions that might complicate the pregnancy. The income limits for pregnancy-related Medicaid vary, but states cannot drop eligibility for this coverage below a legal floor that ranges from an income of 133% to 185% of FPL , depending on the state. States are permitted to set a higher income cutoff.
Childrens Health Insurance Program
Missouri Now Uses A Single Application Form To Apply For Medicaid
There are three broad groups which applicants would fall under which determine how best to apply.
Missouri Medicaid Expansion is effective beginning 07/01/2021.
Helpful links for DMH Agencies and Providers:
- The IM-6AR Appointing an Authorized Representative form should be used if the application has already been submitted and the “Appendix C” was not included with the application.
Disabled Application Flow Chart Please review this flow chart if you will be assisting a DMH consumer with the application process.
Don’t Miss: Is It Ok To Use Vagisil While Pregnant
Medicaid Eligibility And Enrollment: Getting Help With Medicare Costs
July 15, 2021 / 6 min read / Written by Jason B.
The Medicaid program provides financial assistance with health costs for low-income people, including pregnant women, children, disabled people, and older adults. Medicaid eligibility is limited to United States citizens and lawfully present residents who meet federal and state income and residency requirements.
Medicare beneficiaries with limited incomes may also be eligible for the Medicaid program. These individuals can get help paying for Medicare out-of-pocket expenses, such as deductibles, premiums, copayments, and coinsurance.
Note that health care under Medicaid is not necessarily completely free of charge. There may be costs to you, such as copayments details may vary by state.
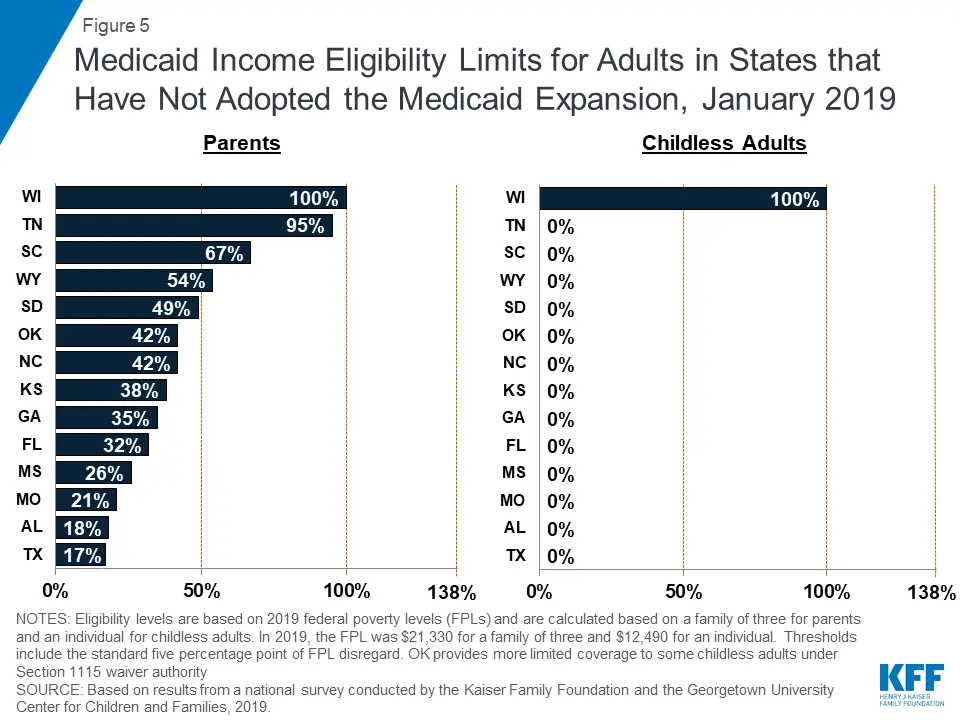
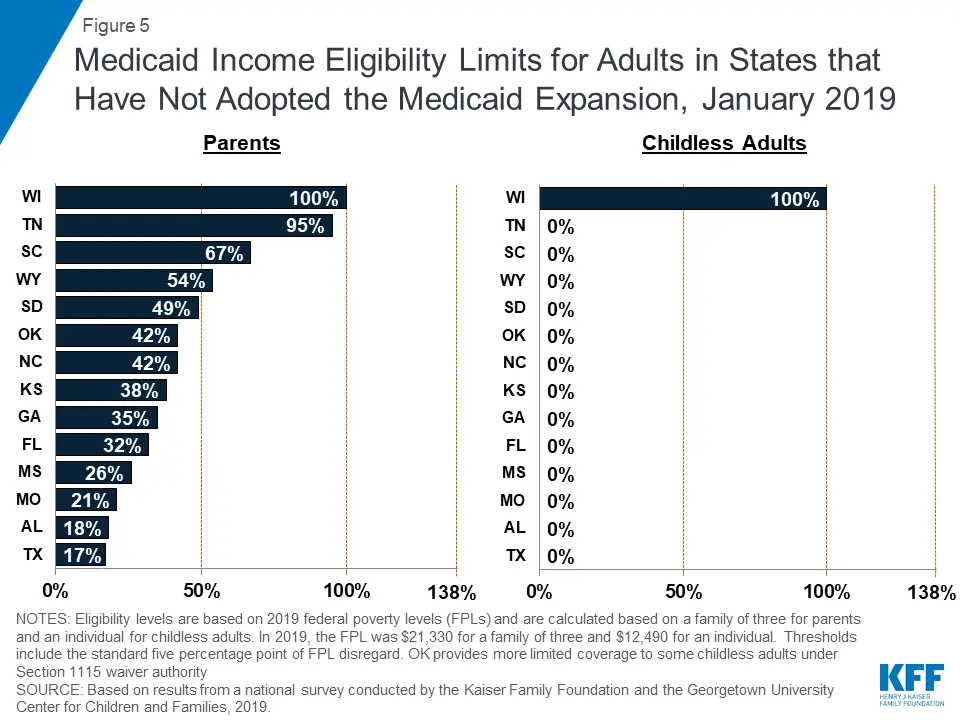
State Medicaid eligibility
The federal government partially funds the program and provides minimum requirements for Medicaid income eligibility. However, each state determines Medicaid eligibility for its residents. The state requirements can vary depending on your income and situation.
Most states determine Medicaid eligibility by income and family size with respect to the Federal Poverty Level .The federal minimum eligibility level was $25,100 for a family of four in 2018. In some states, you might qualify for Medicaid if you earn more than the FPL for the number of people in your household.
Medicaid income eligibility may vary by state. You might qualify in your state even if you dont meet the federal minimum requirement.
Will A Marketplace Health Plan Also Cover A Newborn
Yes. The ACAs EHB requirement mandates coverage of maternity and newborn care. Newborn care covers childbirth and immediate care for the baby after birth. The specifics of this coverage will vary by state and by each individual plan, but all women in Marketplace coverage must also enroll their baby in coverage soon after birth.
If the newborn is eligible for Marketplace coverage, then the parents can choose to add the baby to the familys existing Marketplace plan or choose a new Marketplace plan for the baby. If they opt for the latter, they can enroll the baby into a new Marketplace plan at any metal tier. However, when enrolling a newborn into Marketplace coverage, other members of the household are generally not permitted to change their existing Marketplace coverage.
Don’t Miss: Is Kinesio Tape Safe For Pregnancy
Action Steps For States
- States must add counseling and pharmacotherapy benefits for pregnant women, which under Section 4107 of the Affordable Care Act are now mandatory benefits under Medicaid. This coverage is defined as diagnostic, therapy, counseling services, and pharmacotherapy for cessation of tobacco use by pregnant women. For more information, please see State Medicaid Director Letter #11-007 and contact your regional CMS office.
- Promote cessation benefits to pregnant women and all women of reproductive age.
- Make use of the many resources available to the public and to health care providers to help women quit smoking. See this Resource Guide for a list of highlighted resources.
For technical assistance and additional resources, contact .
How Can I Determine If I Qualify For Medicaid
Qualifying for Medicaid is not as black and white as qualifying for most other government programs. Most government programs have some basic requirements along with very clear income guidelines to help individuals know if they qualify.But Medicaid has many ways that someone can qualifyand even though income makes up part of the eligibility requirements, it is not solely based on that. Even people with the lowest incomes may not qualify for Medicaid if they do not fall into one of the Medicaid groups.
And people who make a middle-range income may qualify if they fit one of the qualifying groups and can fall back on options such as share of cost
If you are pregnant and uninsured, Contact your local Medicaid office to find out if Medicaid is the right option for you.
Compiled using information from the following sources:
1. US Government Information
Don’t Miss: Can I Drink Breakfast Essentials While Pregnant
Does Cigna Health Insurance Cover Pregnancy
While you can get regular health insurance when you are pregnant, you will not be able to get maternity coverage as most companies consider pregnancy a pre-existing condition. This means you will need to undergo a waiting period before availing coverage under a maternity health insurance plan.
Contents
Make Too Much For Medicaid
Women who are pregnant without health insurance and think they make too much money to qualify for Medicaid still have publically funded options that make it affordable to keep your baby.
|
$51,072 |
Medically Needy
Women having a baby without insurance whose household members earn too much money to qualify for Medicaid could become eligible under the medically needy criteria. In this program, large unreimbursed medical expenses could subtract from your earnings and push you under the state income limit.
For example, an uninsured woman with health problems might have significant doctor bills that could wipe out most of her earnings. Keep detailed records to substantiate these expenses to speed possible approval.
Full Scope
Women having a baby without insurance who were ineligible for full-scope or regular Medicaid because their household earnings are too high might want to re-apply or file an appeal. The full-scope version has the strictest qualifying criteria.
Meanwhile, the limited pregnancy-related coverage has much looser eligibility rules for earnings, as illustrated by this simple chart. As you can see, there is a significant increase in allowed salary.
Each state sets income limits based on a percentage of the Federal Poverty Level.
| Lowest % |
|---|
|
Wisconsin |
You May Like: Can You Donate Plasma While Breastfeeding
Does Private Insurance Also Cover A Newborn
It depends. Small group employer-sponsored plans must include the EHBs, including maternity and newborn care, but large group and self-insured employer-sponsored plans are exempt from this requirement. While the requirement for newborn care covers childbirth and immediate care following birth, women must enroll their babies in coverage soon after birth.
What Is Pregnancy Medicaid
Medicaid is a government-sponsored health insurance program for low-income families who have no medical insurance or inadequate insurance. All states offer Medicaid or a program similar to Medicaid to help pregnant women receive adequate prenatal and postpartum care. Medicaid also offers health insurance to seniors, children, and people with disabilities.
Don’t Miss: Can I Use Vagisil Wash While Pregnant
Person Who Is Aged Blind And/or Disabled
Apply if you are aged , blind, or disabled and have limited income and resources. Apply if you are terminally ill and want to get hospice services. Apply if you are aged, blind, or disabled live in a nursing home and have limited income and resources. Apply if you are aged, blind, or disabled and need nursing home care, but can stay at home with special community care services. Apply if you are eligible for Medicare and have limited income and resources.
Pregnant Women And Infants
Healthy Connections provides coverage to pregnant women with low income. This coverage for the mother continues for 60 days after the baby’s birth. The infant is covered up to age one.
A woman who may qualify for this program must:
- Be pregnant
- Be a South Carolina resident
- Be a U.S. citizen or Lawful Permanent Resident Alien
- Have a Social Security number or verify an application for one
Individuals who are eligible will receive all Medicaid covered services.
Apply online or complete the following form and submit it electronically to , by mail to SCDHHS-Central Mail, P.O. Box 100101, Columbia, SC 29202-3101 or to your .
The Omnibus Budget Reconciliation Act of 1986 gave states the option to provide Medicaid coverage to pregnant women with low income.
Also Check: Is It Safe To Take Tums While Pregnant
Who Is Eligible For Medicaid
The general guidelines for eligibility for Medicaid are set by the Federal government however, each state sets up their own specific requirements for eligibility and these can differ from state to state.
All States are required to include certain individuals or groups of people in their Medicaid plan.
The state eligibility groups are:
- Categorically needy
- Medically needy
- Special groups
In the categorically needy group, this will cover pregnant women whose income level is at or below 133% of the Federal Poverty level.
In the medically needy group, this will cover a pregnant woman who makes too much money to qualify in the categorically needy group. This means that women, who may have been denied Medicaid before, may be able to qualify now.
The Tafdc Advocacy Guide Is Out Of Date
Alert
Many of the rules in the guide do not apply right now. See Help with food and cash during COVID-19.
If you are age 20 or older, you are pregnant, and you have no other children living with you, you can get TAFDCfor yourself onlybeginning with your third trimester . If you are a teen , you are pregnant, you have no other children living with you, and you are meeting the teen school attendance requirements, see School attendance rules for teen parents, you can get TAFDCfor yourself onlyas soon as the pregnancy is verified. 106 C.M.R. §§ 703.210 DTA Online Guide .
If you are living with but not married to the babys father, his income should not be counted until the baby is born. 106 C.M.R. §§ 704.235.
You should begin the application process several weeks before your eligibility date in order to get benefits as soon as you are eligible.
Example
Carolyn is pregnant and is due on December 16. She can get TAFDC beginning on August 18 . She should apply in July.
Advocacy Reminders
- A pregnant woman not yet eligible for TAFDC may be eligible for EAEDC cash benefits if she is disabled.
- Pregnant women at any stage of pregnancy may also be eligible for MassHealth SNAP nutrition benefits through the Department of Public Health, 1-800-WIC-1007 and emergency shelter for families through the Department of Housing and Community Development .
Read Also: Why Can’t You Donate Plasma While Pregnant
What Is The Medicaid Program
Good health is important to everyone. If you can’t afford to pay for medical care right now, Medicaid can make it possible for you to get the care that you need so that you can get healthy and stay healthy.
Medicaid is available only to certain low-income individuals and families who fit into an eligibility group that is recognized by federal and state law. Medicaid does not pay money to you instead, it sends payments directly to your health care providers. Depending on your state’s rules, you may also be asked to pay a small part of the cost for some medical services. In general, you should apply for Medicaid if you have limited income and resources. You must match one of the descriptions below:
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your .
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
> >
Don’t Miss: How To Use Nutraburst
How Long Does Medicaid Or Chip Coverage For Pregnancy Last
Medicaid or CHIP coverage based on pregnancy lasts through the postpartum period, ending on the last day of the month in which the 60-day postpartum period ends, regardless of income changes during that time. Once the postpartum period ends, the state must evaluate the womans eligibility for any other Medicaid coverage categories.
7. Is abortion covered by Medicaid or CHIP?
The Hyde Amendment, an annual requirement added by Congress to a federal appropriations bill, prohibits using federal funds abortion coverage except when a pregnancy results from rape or incest, or when continuing the pregnancy endangers the womans life. However, states may use their own funds to cover abortions, and 17 states currently do.
Medicaid Letters: Medicaid And Pregnancy
What is Medicaid?
Medicaid is a health insurance program for low income people. It pays most medical costs, including hospital care, doctors visits, prescriptions and prenatal care.
Is there a special Medicaid program for pregnant women?
Yes. It is important for pregnant women to get medical care as early in their pregnancy as possible. Medicaid has a special program called Presumptive Eligibility, which pays for medical care for pregnant women before their Medicaid applications have been approved.
To find out if you are eligible for Presumptive Eligibility, call one of the clinics on the list we have enclosed. People at the clinic can tell you if you qualify. If you do, you can immediately receive medical assistance. The Department of Social Services will make a decision within 45 days of the 1st medical appointment/application being placed.
Is it easier to get Medicaid when I am pregnant?
Yes. Because it is so important for pregnant women to get medical care, you are allowed to earn more money than other people. This is called Expanded Eligibility. Even if you have been denied regular Medicaid, you may be eligible under the expanded eligibility income levels. Any of the qualified clinics can tell you if you are eligible. Contact one of them.
What happens if I am presumptively eligible for Medicaid?
Remember, to be eligible for ongoing medical care you must complete your application for regular Medicaidduring your 45-day period of presumptive eligibility.
BATAVIA OFFICE
You May Like: Can I Use Vagisil Wash While Pregnant
Get Important News & Updates
Sign up for email and/or text notices of Medicaid and other FSSA news, reminders, and other important information. When registering your email, check the category on the drop-down list to receive notices of Medicaid updates check other areas of interest on the drop-down list to receive notices for other types of FSSA updates.
Related Questions Answered On Yanswers
- Do you have to be married for tricare insurance to cover you?
- Q: My boyfriend and i have been dating for almost two years and we kinda had an oops. and im eighteen weeks pregnant. well medicade wont cover me because i havent had my greencard for over five years. and my insurance wont cover a teen pregnancy. and the bills are almost impossible to pay. its 500 a month just for the OBGYN and 20,000 for the birth without an epidural with only a year to pay that off. my boyfriend is in the army. hes still in some training right now to be a ranger and we know that his insure would cover the maternity expenses if we were married but weve heard that i could be covered without us being married because its his child. but we cant get clear answers from anyone.so if you know much about this insurance and how it works it would greatly be appreciated.
- A: You have to be married for TriCare coverage. The military does not recognize Common Law marriages or domestic partners unless they are legally married. Besides you boyfriend will get extra money for dependents, possibly housing allowance, and food allowance. I dont know where you got your figures on pregnancy and delivery costs, but they are waaaaaaaaaaay to high. So in order for good medical coverage, you need to get married.
Also Check: Can You Use Vagisil During Pregnancy
Tenncare Income Limit For Pregnant Women/newborns
| Household Size* |
|---|
|
$7,258 |
* A pregnant woman is generally counted as a household of two .
To sign up for presumptive eligibility, just go to your local health department. They can enroll you.
Even if you get temporary TennCare, you will need to fill out the full application.
You can apply for TennCare at tenncareconnect.tn.gov.
Need help applying? There are at least three ways that you can get help:
If you have a disability, someone can even come to your house to help you apply for TennCare. Just call your local Area Agency on Aging and Disability at 1-866-836-6678.
More information about eligibility.
