Health Plan Report Cards
People across Texas shared their thoughts about their health plan, and rated them, one to five stars, on the services their plan provided.You can compare plans using the overall ratings or by looking at the services that matter the most for you and your family.
You can view the report cards on the Managed Care Report Cards page. Click the program you are enrolled in and find your service area to see plans available to you.
Changes In The Senate
While presenting the Senate version of House Bill 133 to her colleagues in the upper chamber, state Sen. Lois Kolkhorst, R-Brenham, defended the shortened extension.
The media has portrayed our version of this, as cutting it from 12 to six, said Kolkhorst, who also sponsored the bill. I want to make sure that we clarify that we are adding four months, and we will become one of the first states in the nation to extend it beyond two months.
Aside from extended postpartum care, provisions the Senate added to HB 133 include transitioning case management services for children and pregnant women on Medicaid and in the Healthy Texas Women program to managed care. The state plans to move away from a fee-for-service model to contracting with managed care organizations that work with a certain network of providers.
Ramirez said that could mean better service for women experiencing postpartum issues, but the real impact of the change remains to be seen. Thats especially true for traditional family planning providers that may not have much experience working with managed care organizations.
Adriana Kohler, a policy director with the childrens policy nonprofit Texans Care for Children, said that although HB 133 is set to go into effect on Sept. 1, it could still take a while to see the actual benefits play out because it will take time for state and federal officials to secure funding.
Texas Medicaid Application And Qualifications
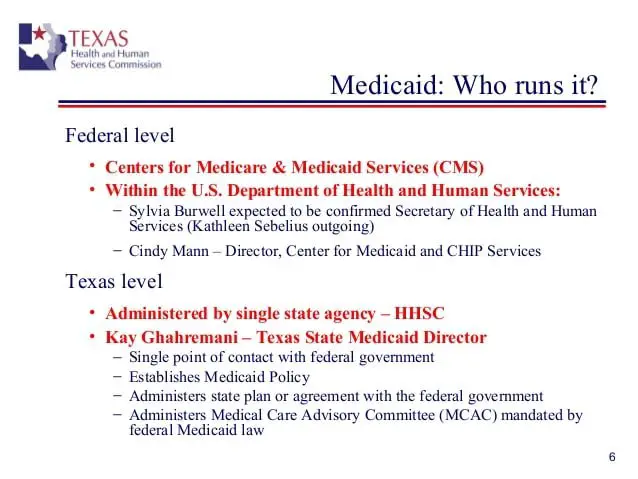
It is easy to confuse Medicaid with Medicare. The two programs are not without their similarities. One key difference is that Medicare is a federal program, whereas Medicaid is a state program with rules that vary depending on where you are. The other major difference is that Medicare is based largely on age and disability, while Medicaid is based largely on income.
Depending on your circumstances, you can be on both at the same time. Circumstances is the key word. Medicare tends to be long-term, if not permanent. Medicaid is often a shorter-term solution. There are other programs that are generally associated with Medicaid such as financial and grocery assistance. It is possible that if you have qualified for these other forms of assistance, Medicaid will be included.
Also Check: Vagisil Safe While Pregnant
Who Can Be A Provider
Physicians, community clinics and providers who offer prenatal care within their scope of practice can provide CHIP perinatal prenatal care. This includes obstetricians/gynecologists, family practitioners, general practitioners, nurse practitioners, internists, nurse midwives or other qualified health care providers.
Those who can provide CHIP perinatal care for newborns are the same types of providers as traditional CHIP.
CHIP perinatal care is provided by all CHIP health plans throughout the state. Health plans recruit physicians and providers for their respective networks. To become part of a network, physicians and providers must meet requirements of the respective health plan, such as credentialing standards, and have a contract with the health plan.
Effective Date Of Coverage
Once an individual is determined eligible for Medicaid, coverage is effective either on the date of application or the first day of the month of application. Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Read Also: Vagisil When Pregnant
How Do I Know If An Applicant I Have Treated Is Enrolled In Healthy Texas Women And Her Claim Will Be Paid
To see if a woman is enrolled in the program:
- Check in the Texas Medicaid Provider section of the Texas Medicaid & Healthcare Partnership website. .
Providers should make sure that a woman is enrolled in the program before billing. Claims received before enrollment will be denied, but providers can resubmit claims once a woman is enrolled. Providers have 95 calendar days from service delivery to bill the program.
How Are Providers Reimbursed What Are The Reimbursement Rates
To be reimbursed, providers must participate in a health plan’s network. Reimbursement rates will be negotiated between the provider and the health plan per contractual agreements. Providers will submit claims directly to the health plan for payment. Claim forms and processes vary by health plan. Consult the CHIP perinatal health plan for billing details.
Don’t Miss: Nutraburst Side Effects
What If A Client Needs To Report A Change To Her Case
Report changes on Form H1019, Report of Change. The form is available in English and Spanish.
- Clients do not have to submit a copy of their Social Security cards, and the card cannot be used as proof of citizenship or identity.
- If the woman changed her name legally but did not report the change to the Social Security Administration, she can visit the Social Security Administration website to find out how to change or correct the name on her card.
Can A Pregnant Woman Be Denied Medicaid In Your State
Medicaid can deny coverage to pregnant women for several reasons. Learn about the guidelines before completing an application to avoid needless rejection.
Medicaid is a publicly-funded program designed to act as a safety net for low-income families, disabled individuals, senior citizens with few resources, and pregnant women.
The government must have a cutoff point because it cannot offer taxpayer-supported benefits to every applicant. Household income levels compared to size and citizenship status are the two primary eligibility criteria.
As always, the devil is in the details. Pay close attention to boost your approval odds.
Also Check: Can You Take A Tums While Pregnant
Apply For Medicaid In Texas
You can enroll through HealthCare.gov or the state Medicaid website. You can enroll by phone at 800-318-2596.
Eligibility: The aged, blind, and disabled. Also, parents with dependent children are eligible with household incomes up to 15% of FPL. Children are eligible for Medicaid or CHIP with household incomes up to 201% of FPL, and pregnant women are eligible with household incomes up to 198% of FPL.
When You Really Really Really Need It Youre Denied
How Texas came to have the worst insurance gaps in the country is no mystery: It was an accumulation of deliberate policy choices by state lawmakers going back decades, driven largely by an aversion to government-mandated insurance and a desire to keep taxes low.
The design of our entire system is to be very limited, and historically we are very distrustful of government in general, said Texas Rep. Sarah Davis, a Houston Republican who chairs the House Appropriations Subcommittee on Health and Human Services. Dr. Amy Raines-Milenkov, a University of North Texas Health Science Center professor and member of the states maternal mortality review committee, believes the states culture of personal responsibility leads it to abandon its most vulnerable. We dont have the belief here that people should have access to health care, she said. Even the safety nets are built on keeping people out rather than pulling people in.
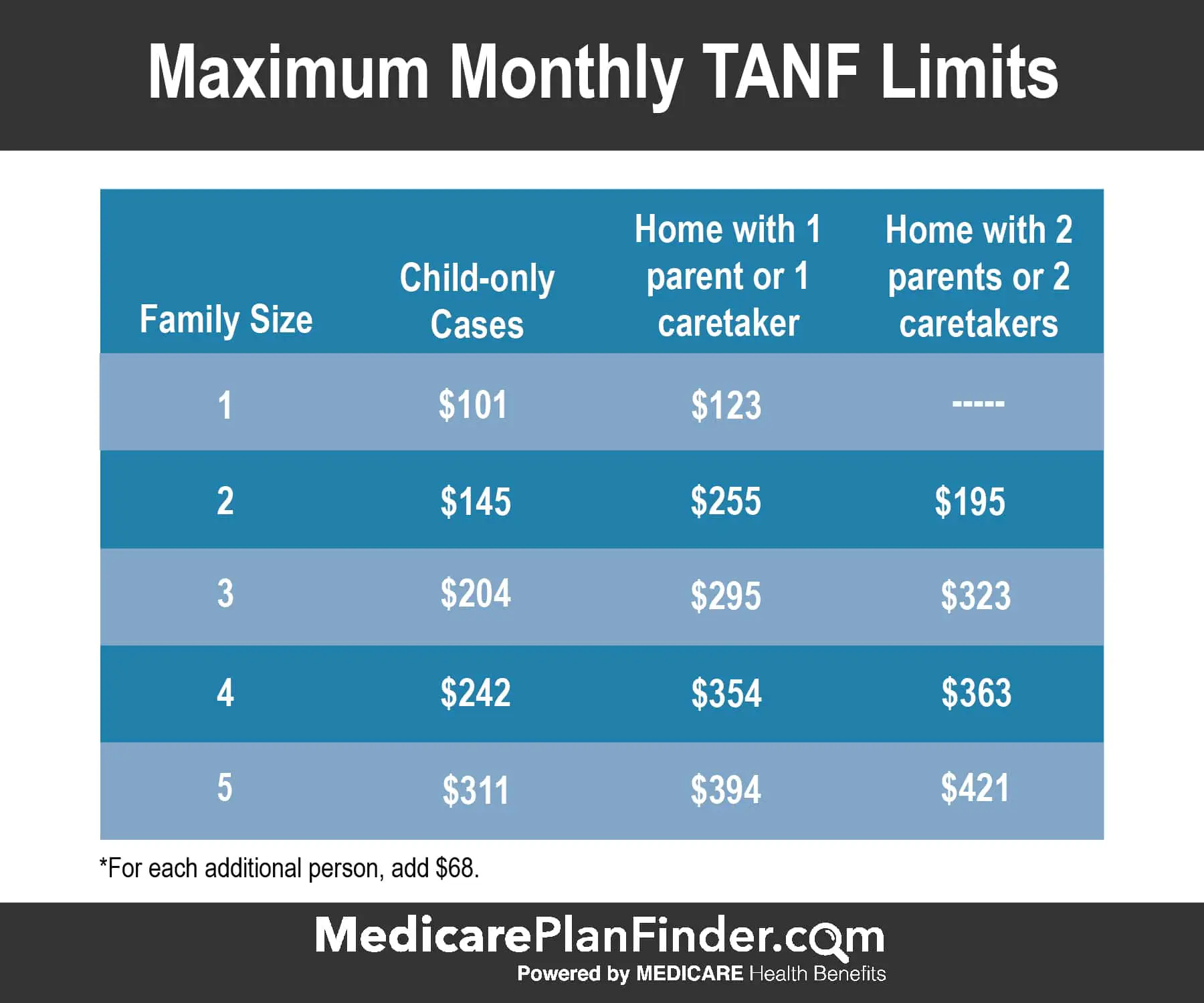
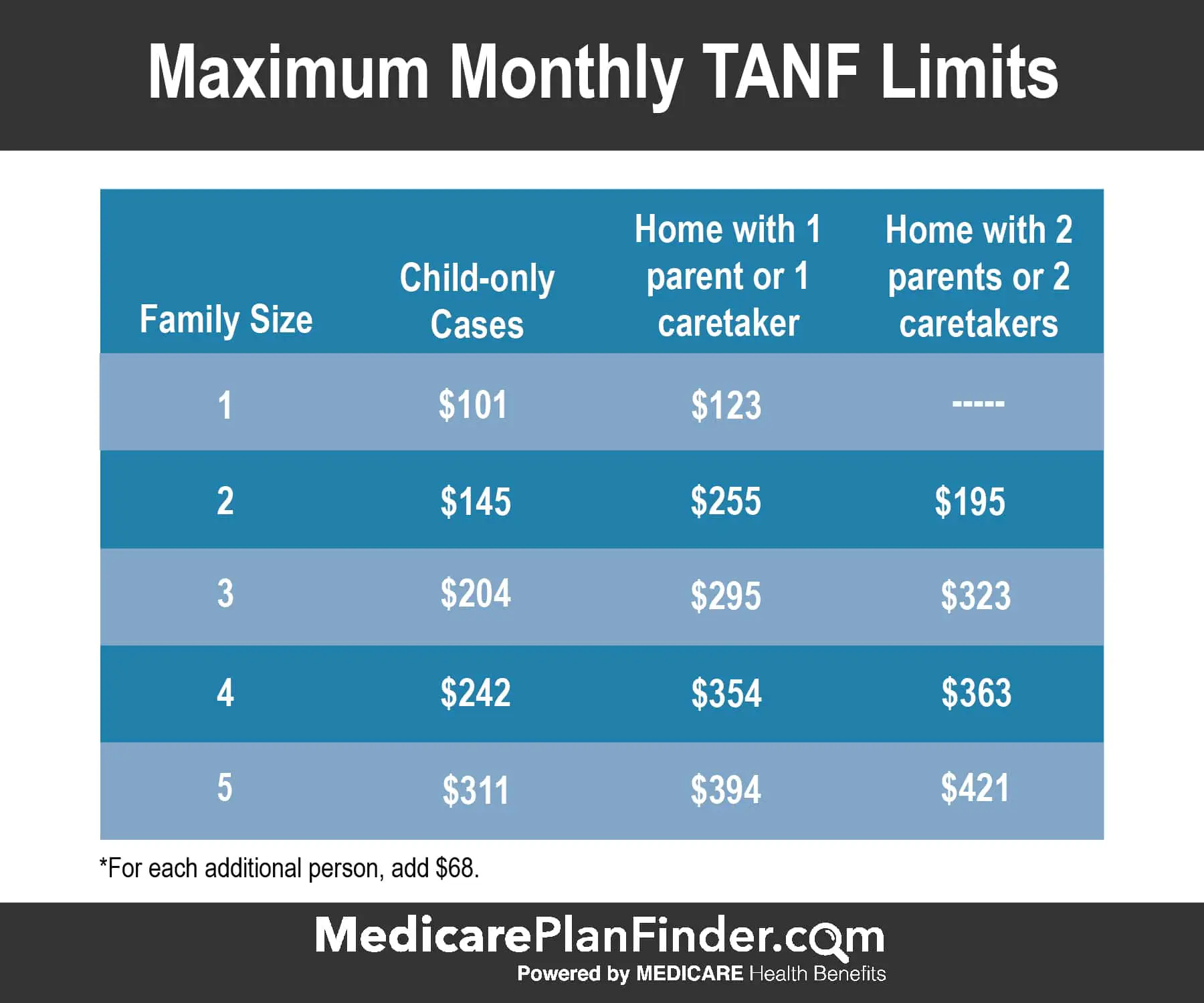
People who dont have children or disabilities cant receive Medicaid, no matter how poor they are. A single mother with two children only qualifies if she earns the equivalent of 17 percent of the federal poverty level or less $230 to $319 per month, depending on whos doing the calculation.
But after the US Supreme Court ruled that states couldnt be forced to accept the Medicaid expansion, Texas became one of 14 states that opted not to a decision that has denied coverage to 1.4 million Texans who would have otherwise qualified for insurance.
You May Like: Can You Have Lasik While Pregnant
How To Apply For Medicaid
Enter your zip code to get started.
Texas Medicaid provides medical coverage provide necessary medical benefits to residents of Texas. The low-income families can receive comprehensive health coverage through Medicaid program. The program is a joint venture between state of Texas and federal government.
Texas Medicaid is available for elderly, living single or married and living together. The eligibility criteria for single and married elders are different. Financial criteria are also different for single and married couples.
Texas Medicaid program provides various medical benefits to enrollees. These benefits include medical home, continuity of care, and other basic health benefits. The program provides comprehensive health care for qualified members of community.
If you are receiving SSI income or you qualify for Temporary Aid to Needy Families, you will automatically qualify to receive health coverage through Texas Medicaid program.
Pregnant women with income at or below 185% will be eligible to receive aid through Texas Medicaid program.
In order to apply online for Texas Medicaid benefits, you can visit Texas Benefits website. You can also apply in person by visiting HHSC office near you.
If You Dont Have Health Coverage
- Health coverage makes it easier to get the medical check-ups and screening tests to help keep both you and your baby healthy during pregnancy.
- If you qualify for a Special Enrollment Period due to a life event like moving or losing other coverage, you may be able to enroll in a Marketplace health plan right now. Being pregnant doesnt make you eligible, but the birth of a child does.
- Create an account now to apply for Marketplace coverage through the Open Enrollment Period or a Special Enrollment Period. If you select the option to get help paying for coverage on your application, youll be asked if youre pregnant. Reporting your pregnancy may help you and your family members get the most affordable coverage.
- If you dont qualify for a Special Enrollment Period right now, youll be eligible to apply within 60 days of your childs birth. You can also enroll in 2021 coverage during the next Open Enrollment Period this fall.
- If eligible for Medicaid or CHIP, your coverage can begin at any time.
Recommended Reading: Pregnancy Side Effects Week By Week
How Do I Enroll In Medicaid In Texas
If you believe you may be eligible to enroll in Medicaid in Texas:
- You can enroll through HealthCare.gov, either online or by phone at 1-800-318-2596.
- You can enroll through the Medicaid website maintained by the Texas Health and Human Services Commission.
- You can also download and print a paper application, or request that one be mailed to you, by using this page on the Texas Medicaid website.
If You May Qualify For Medicaid Or Childrens Health Insurance Program
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
Recommended Reading: Vagisil Cream While Pregnant
What Other Documents Do Women Need To Send With Their Application
Women applying for CHIP perinatal services need to submit the following documents of proof:
Proof of Income
Proof must show current income for each person in the home. Proof can be:
- Pay check stub from the last 60 days showing pay before taxes or deductions
- Last year’s tax return
- Proof of self-employment
- Letter from your employer. This letter takes the place of a paycheck stub. It should how much you make now and how often you get paid. It also should include your name, the employer’s name, and the employer’s signature.
- Social Security statement
Austin, TX 78714-9968
In person
Finished applications and copies of required information can be turned in to a local HHS benefits office. To find the office nearest you, call 2-1-1 or 877-541-7905 after you pick a language, press 2.
Does Enrollment In Healthy Texas Women Affect Other Texas Health And Human Services Benefits
A woman’s enrollment in Healthy Texas Women does not make a household ineligible for other program benefits such as Medicaid, TANF or SNAP. But the information reported when applying for Healthy Texas Women might affect the household’s other benefits if it’s different than what was previously reported for other programs.
Don’t Miss: Why Can’t You Donate Plasma While Pregnant
Who Can Get Medicaid In Texas
You should apply for Medicaid if your income is low and you match one of the descriptions below:
- You think you are pregnant
- The parent or caretaker of a child and/or teenager under the age of 19.
- You are a child or teenager age 18 or under.
- An adult age 65 or older.
- You are legally blind.
- Living with a disability or disabled.
- You are in need of nursing home care.
How To Choose A Health Plan
When picking a plan, think about the following:
- Are doctors you already use and like covered by the plan?
- How is the plan rated on issues that are important to you and your family?
- What value-added services are available through the plan?
We also provide tools to help you choose the best plan for you and your family.
You May Like: Can A Pregnant Woman Take Tums
Texas Has A Program For Pregnant Noncitizens But The Program Doesnt Actually Care For Them
There is one category of patients who pose a particular conundrum for obstetric providers in Texas: immigrants. The state has the highest number of births to noncitizens outside of California, and many of those women are low-income. The large majority cant access pregnancy Medicaid, even though most other states allow longtime legal residents to participate.
Texas does have a prenatal care program for noncitizens. Theres a huge caveat, however: It doesnt actually cover the mother, just the fetus she is carrying. It may be the ultimate example of the states fragmented maternal care system and how that system prioritizes babies.
The program dates back to President George W. Bush, who extended the Childrens Health Insurance Program to cover unborn babies. At the time, the idea the fetus is a child and a future citizen and should therefore receive prenatal care attracted more attention for its anti-abortion origins than for its potential to help immigrant mothers. In many of the 16 states that have adopted it, the type of care women receive isnt much different than what they would get under pregnancy Medicaid.
Related
California decided it was tired of women bleeding to death in childbirth
Some of the programs biggest limitations come after the baby has been delivered. While new mothers get two routine checkups, those whose needs are not routine must fend for themselves.
How Long Does The Eligibility And Enrollment Process Take
Texas Health and Human Services staff have 15 business days to process the application from the day they received it. Once eligibility is determined, the pregnant woman enrolls in a CHIP perinatal health plan on behalf of her unborn child. She has 15 calendar days to select a health plan from the day she gets a letter stating she can get CHIP perinatal benefits. If she does not choose a medical plan within the 15-day timeframe, HHS will choose one for her.
Also Check: Can I Use Vagisil Cream While Pregnant
Can Women With Health Insurance Coverage Enroll
Women enrolled in Medicaid, CHIP or Medicare Part A or B are not able to get Healthy Texas Women. A woman who has private health insurance is not eligible for the program unless:
- her private insurance does not cover family planning services or
- filing a claim on her health insurance would cause physical, emotional or other harm from her spouse, parents or other person.
How Can Pregnant Women Apply
Providers who want to have applications available in their office can order them can order them online. The application is named Application for Health Coverage & Help Paying Costs the form number is H1205.
Women can apply for coverage online at YourTexasBenefits.com or apply by phone, mail, or fax. Learn more about these other ways to apply.
All applicants for CHIP perinatal services will be screened to see if they qualify for Medicaid for Pregnant Women. If they don’t qualify for Medicaid, HHS will determine if they qualify for CHIP perinatal coverage.
Don’t Miss: Vagisil Cream Pregnancy
Mothers Find Their Own Stopgaps In The Face Of Crisis
The urgent need to fix the gaps in postpartum care has captured the attention of national reformers, who see it as a critical step toward narrowing racial disparities in maternal mortality. Several 2020 Democratic presidential candidates have proposed federal legislation to extend pregnancy Medicaid to a full year postpartum, and state lawmakers have introduced a wave of similar bills. Missouri passed a limited extension last year and Illinois a far more sweeping one this past July both plans are awaiting federal approval.
The enthusiasm extended to Texas, where a broad coalition, led by the maternal mortality review task force, came together this past legislative session to support a full-year extension. The effort passed the House but stalled in the Senate. All the oxygen in the room this session was taken up by school finance reform, the legislative priority of the states top Republicans, said Tim Schauer, an Austin-based lobbyist on womens health issues.
The five-year cost of extending postpartum coverage was estimated at nearly $1 billion in state and federal funds, according to Politico. Rep. Shawn Thierry , who introduced one of the extension bills, had to counter skeptics who thought that the states alarming maternal mortality numbers were, as she said, kind of a hoax and that increasing benefits for new mothers was just a stealth tactic aimed at expanding Medicaid more widely.

