Tennessee Medicaid Income Limit
The Tennessee Medicaid Income Limit is calculated as a percentage of the Federal Poverty Line.
To qualify, you must meet the Tennessee Medicaid Income limits listed below.
Here is the Federal Poverty Level for 2021.
| 2021 Federal Poverty Levels for the 48 Contiguous States & D.C. |
| Household Size |
Additionally, to be eligible for Medicaid, you cannot make more than the income guidelines outlined below:
- Children up to age 1 with family income up to 195 percent of FPL
- Any child age 1-5 with a family income up to 142 percent of FPL
- Children ages 6- 18 with family income up to 133 percent of FPL
- CHIP for children with family income up to 250 percent of FPL
- Pregnant women with family income up to 195 percent of FPL
- Parents of minor children with family income up to 96 percent of FPL
- Individuals who are elderly, blind, and disabled with family income up to 74% of the FPL
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
Medicaid Expansion In Tennessee
Tennessee has not expanded Medicaid coverage as allowed under the Affordable Care Act, which means that there are an estimated 117,000 residents in the coverage gap ineligible for Medicaid and also ineligible for premium subsidies in the exchange. This group is comprised of non-disabled adults with income below the poverty level and without minor children.
Federal
0.0%
of Federal Poverty Level
But Medicaid expansion in Tennessee has been a non-starter for most Republican lawmakers, and the GOP holds a strong majority in both chambers of the states legislature. Instead, GOP lawmakers voted in 2018 to impose a work requirement on low-income parents who are currently eligible for Tennessee Medicaid. They propose using TANF funding to cover the cost of implementing the work requirement.
Tennessee also enacted legislation in 2019 to seek federal permission for a block grant funding model for Medicaid an approach that Congress rejected in 2017, but that Republican lawmakers have long supported. The states block grant funding proposal was approved by the Trump administration in its waning days, although changes might be made under the Biden administration.
In addition, 128,000 children have been removed from the Tennessee Medicaid program in some cases because they were no longer eligible, but in others because of missing or erroneous paperwork.
Recommended Reading: Can I Put Braces While Pregnant
Has Your Social Security Payment Been Cut And You Dont Know Why
You may have been getting help paying your premiums and other costs from a Medicare Savings Program that is no longer in effect. With an MSP, TennCare was actually paying your premiums for you. But, each year you need to renew your MSP through a process called redetermination. People can lose their coverage for several reasons including:
- Their income is too high.
- Have too many resources like cars, land or money in the bank.
- Not returning the packet to TennCare by the deadline.
We may be able to help! Simply give us a
Additional Factors For Determining Medicaid Eligibility In Tennessee
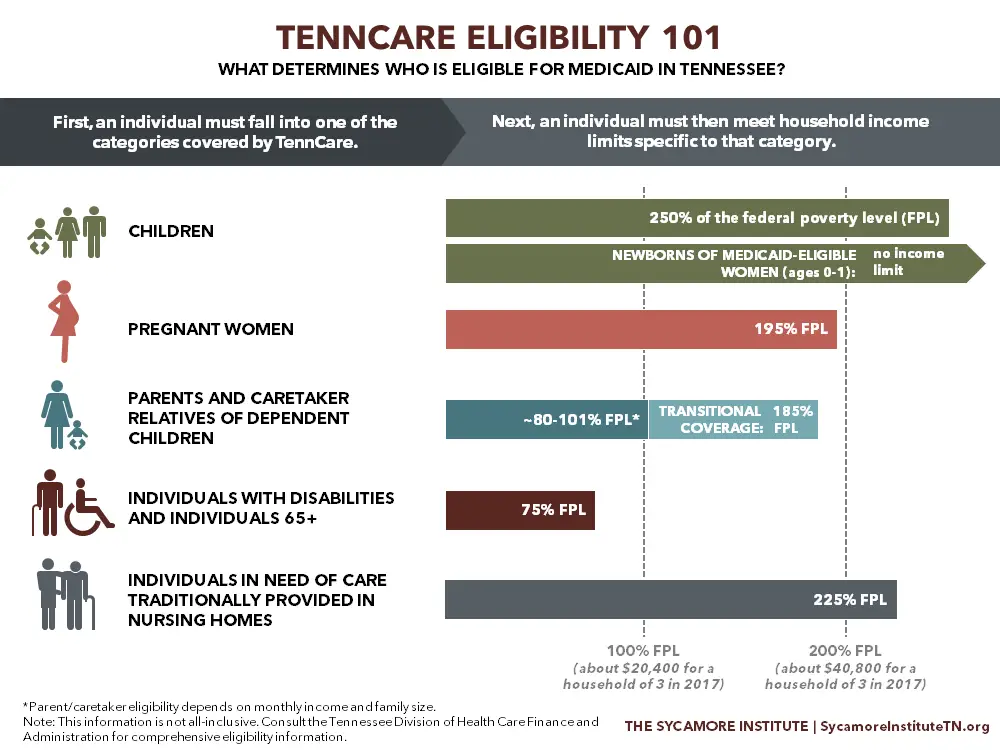
TennCare also has other eligibility categories that are not pictured, and some categories have additional criteria for determining eligibility. For example:
- In addition to income limits, some eligibility categories also have resource limits. Low-income individuals ages 65+, for instance, can have no more than $2,000 in resources and assets to qualify for full TennCare coverage.
- TennCare covers uninsured women with household incomes below 250% of FPL and have had breast or cervical cancer detected by the Tennessee Breast and Cervical Cancer Screening Program. While not publicly available, enrollment numbers for this category are likely relatively low. From 2011 to 2015, the screening program detected about 970 cases of breast and cervical cancers and premalignant lesions.
Comprehensive information about TennCare eligibility can be found on the states website:
You May Like: Is It Bad To Donate Plasma While Pregnant
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
How To Apply For Aged Blind Or Disabled Medicaid Benefits
If you are applying for aged, blind or disabled Mississippi Medicaid benefits and services, an in-person interview may be required. If so, you will be contacted by staff at the regional office that serves your county of residence.
- Apply by filling out the Mississippi Medicaid Aged, Blind and Disabled Application Form and submitting the application to the regional office that serves your county of residence or if the applicant is in a nursing home, the regional office that serves the county where the nursing facility is located. Mail or bring in the application at the time of the in-person interview if one is required. It is advised that you do not email forms or submit online forms with protected health information or personally identifiable information, to protect your confidentiality in accordance with the Health Insurance Portability and Accountability Act of 1996.
Read Also: Can I Take Tums While Pregnant
Who Is Eligible For Tennessee Medicaid
Because Tennessee has not yet expanded Medicaid under the ACA, eligibility guidelines are unchanged from 2013, and non-disabled, non-pregnant adults without dependent children are ineligible for Medicaid, regardless of their income. TennCare is available to the following legally-present Tennessee residents, contingent on immigration guidelines:
- Adults with dependent children, if their household income doesnt exceed 103 percent of poverty. This is one of the highest thresholds in the country among states that have not expanded Medicaid.
- Pregnant women and infants under one, with household income up to 195 percent of poverty.
- Children age 1 5 with household income up to 142 percent of poverty, and children 6 18 with household income up to 133 percent of poverty.
- CHIP is available to children with household incomes too high for Medicaid, up to 250 percent of poverty.
Eligibility Levels For Coverage Of Pregnant Women In Medicaid And Chip
This National Academy for State Health Policy map provides eligibility levels for states Medicaid and Childrens Health Insurance Program coverage for pregnant women. Please see the accompanying chart for eligibility levels for states coverage in 2013, 2015, and 2017. Coverage levels for 2015 and 2017 include states modified adjusted gross income-converted eligibility levels. Every state provides pregnancy-related Medicaid coverage to pregnant women at income levels above the historic Aid to Families with Dependent Children levels in place on May 1, 1998. Pregnancy-related Medicaid coverage is mandatory for women earning up to 133 percent of the federal poverty level , but some states provide optional coverage up to or exceeding 185 percent of FPL. States that opt out of these higher Medicaid coverage levels are also allowed to cover pregnant women through CHIP. Under CHIP, states also have the option to provide services to pregnant women through the CHIP unborn child coverage option, which may offer a more limited benefit package.
This chart is based on the information collected by NASHP from multiple sources. To learn more about some of the eligibility and enrollment policy considerations related to pregnant womens coverage, explore these NASHP infographics that depict coverage options for pregnant women.
You May Like: Vagisil When Pregnant
Were You On Tenncare Or Coverkids And Lost It
Chances are you lost your coverage through the annual renewal process called, redetermination. People can lose their coverage for several reasons including:
- No longer qualifying for a program due to their age or the age of a child in their home.
- Their income is too high.
- Have too many resources like cars, land or money in the bank.
- Not returning the packet to TennCare by the deadline.
We may be able to help! Simply give us a .
Tennessee Receives Cms Approval For Block Grant Medicaid Funding
In January 2021, just days before the end of President Trumps presidency, CMS announced that Tennessees Medicaid block grant waiver proposal had been approved. The waiver approval, which is valid for ten years , will allow Tennessee to be the first state in the nation that utilizes a block grant approach to federal Medicaid funding, although Puerto Rico has long used a block grant funding model for Medicaid, which has led to significant funding shortfalls in the territorys Medicaid program.
The incoming Biden administration may make changes to the approved waiver, but they would have to go through a review process. Its noteworthy that law professor Nicholas Bagley pointed out in 2019 that Tennessees proposal was likely not legal under the existing rules for Medicaid and the constraints of what can and cant be changed with 1115 waivers.
In May 2019, Tennessee Governor Bill Lee signed H.B.1280 into law. The legislation directed the state to seek federal permission to convert the states current federal Medicaid matching funds into a block grant, indexed for inflation and population growth. The Trump administration had expressed willingness to consider such proposals, but Tennessee was the first state in the nation to enact legislation to get the ball rolling on it .
You May Like: Pregnant Take Tums
What To Do If You Don’t Qualify For Medicaid
If you don’t qualify for Medicaid, you can possibly get subsidized health care through the Obamacare marketplaces during a special enrollment or open enrollment period. Americans who make between 100% and 400% of the FPL qualify for a premium tax credit that can significantly lower the cost of a plan.
Federal open enrollment for 2019 health care plans ended on Dec. 15, 2018, though some state exchanges are open longer and Nevada sells health insurance all year round. Learn 2020 open enrollments dates by state. Healthcare.gov, the federal exchange, usually opens from November 1 to December 15 each year.
If you can’t find affordable health care on your marketplace during open enrollment, you have a few back-up options.
These include:
Short-term health insurance: Originally designed to prevent short-term health insurance gaps, these plans are cheaper, but much less comprehensive than traditional coverage. They don’t have to cover Obamacare’s ten essential benefits or pre-existing conditions. Following changes by the Trump administration, short-term health plans can last from three months to potentially three years.
Limited benefit plans: These plans cover a very small portion of the costs associated with certain “medical events”, like a doctor’s visit or ambulance ride. Both the number of events and dollar amounts covered are capped.
District Of Columbia Medicaid

Eligibility overview: Washington, D.C., has one of the most generous Medicaid programs in the U.S., covering adults with household incomes up to 210% of the FPL as part of its expansion program. It also has programs for pregnant, parent/caretaker, elderly, disabled and child residents.Income requirements: The expansion covers adults without dependents who make up to $2,082 a month when applying on their own. Elderly, blind or disabled D.C. residents are eligible if they make up to 100% of the FPL, or $1,063 per month for one individual, and have resources below $4,000 for one person. D.C. also covers pregnant women with incomes up to 319% of the FPL, or $3445 monthly, and parents/caretakers with incomes up to 216% of the FPL.
How to apply for Washington, D.C. Medicaid: You can apply online at DC Health Link or by visiting your closest Income Maintenance Administration Service Center.
Other notable programs: Long-term care and nursing home care services Spend Down, a Medicaid program for people who exceed income limits, but have high medical bills Emergency Medicaid for people who canât qualify for standard Medicaid due to citizenship/immigration status.
You May Like: Is It Safe To Eat Tums While Pregnant
Unitedhealthcare Connected Benefit Disclaimer
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® Member Handbook. Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year.
You can get this document for free in other formats, such as large print, braille, or audio. Call , TTY 711, 8 a.m. – 8 p.m., local time, Monday – Friday . The call is free.
You can call Member Services and ask us to make a note in our system that you would like materials in Spanish, large print, braille, or audio now and in the future.
Language Line is available for all in-network providers.
Puede obtener este documento de forma gratuita en otros formatos, como letra de imprenta grande, braille o audio. Llame al , TTY 711, de 08:00 a. m. a 08:00 p. m., hora local, de lunes a viernes correo de voz disponible las 24 horas del día,/los 7 días de la semana). La llamada es gratuita.
Puede llamar a Servicios para Miembros y pedirnos que registremos en nuestro sistema que le gustaría recibir documentos en español, en letra de imprenta grande, braille o audio, ahora y en el futuro.
Los servicios Language Line están disponibles para todos los proveedores dentro de la red.
Tennessee Medicaid Enrollment Numbers
During the first open enrollment period 83,591 people in Tennessee enrolled in Medicaid or CHIP through HealthCare.gov. TennCare requested an additional $180 million from the state in late 2013 because of the rapidly increasing enrollment they were seeing soon after open enrollment began on the exchange.
As of August 2016, TennCare was covering 1.55 million people in Tennessee. A total of 1,628,196 people had coverage through Tennessees Medicaid and CHIP programs as of July 2016. That was a 31 percent increase since the end of 2013, despite the fact that the state had not expanded Medicaid. This is known as the woodwork effect, as people who were already eligible for Medicaid under the existing guidelines come out of the woodwork thanks to the outreach and enrollment efforts under the ACA.
Enrollment in Tennessees Medicaid/CHIP coverage fell sharply since 2016 amid the states efforts to purge children from the coverage rolls . As of February 2019, total enrollment stood at just over 1.3 million people enrolled as of February 2019.
As of June 2020, Tennessee Medicaid and CHIP enrollment was 1,489,536.
Read Also: Can You Get Lasik Eye Surgery While Pregnant
How To Get Temporary Tenncare Right Now
If you are pregnant, you may be eligible to get temporary TennCare right now. This is called presumptive eligibility. This will cover your visits to the doctor and other medical services while you are pregnant.
You can enroll if your income is under the limit in the table below. You must live in Tennessee and you must be a U.S. citizen or eligible immigrant.
How Do I Enroll In Medicaid In Tennessee
Enrollment in TennCare is year-round you do not need to wait for an open enrollment period if youre eligible for Medicaid
- Tennessee uses the federally-run insurance marketplace, so you can enroll through HealthCare.gov or use their call center at 1-800-318-2596.
- You can enroll online via TennCare Connect.
- You can go to any of the states 95 Department of Human Services offices to apply in-person. You can also use the find local help link on HealthCare.gov to find someone in your community who can help you enroll.
- You can print a paper application and submit it to your local Department of Human Services office .
Prior to 2019, the only way to enroll online was through HealthCare.gov. But after five years of delays, Tennessee debuted their TennCare Connect system in March 2019. The new program allows applicants to determine eligibility, enroll, and manage benefits online.
TennCare had initially planned to build a new system that would be functional by October 1, 2013. But that didnt work out, and the old system didnt have the functionality to be upgraded properly. So the state spent several years building the new system.
Recommended Reading: Tums While Pregnant
How Medicaid Eligibility Is Determined
Income eligibility is determined by your modified adjusted gross income , which is your taxable income, plus certain deductions. Those deductions include non-taxable Social Security benefits, individual retirement contributions and tax-exempt interest. For most people, MAGI is identical or very close to your adjusted taxable income, which you can find on your tax return. Specific income requirements in dollars rise alongside the size of your household.
Our guide focuses on each stateâs major programs for adults. Most are only available to state residents, U.S. citizens, permanent residents or legal immigrants .
Looking for insurance for a child? Check out our guide to the Children’s Health Insurance Program .
Medicaid Eligibility In Tennessee
To date, the US government Medicaid program provides free or affordable healthcare coverage to more than 60 million citizens and immigrants nationwide. The Medicaid program was designed to help low-income families and individuals obtain affordable healthcare coverage. Funded both by the state and federal government, each city has their own set of guidelines for eligibility. If you or your family are looking to apply for affordable health benefits, continue reading for state-specific information for Tennessee.
The state of Tennessee offers Medicaid benefits to its residents. Known as TennCare, the state provides opportunities for eligible applicants to receive vital medical services that can include emergency or intensive care, dental care, lab work, eye care, doctors visits, and more.
You May Like: Can You Use Vagisil During Pregnancy
