Preventing Thrombocytopenia In Pregnancy
Prevention of thrombocytopenia during pregnancy is reduced to the exclusion of factors provoking the dysfunction of the immune system of a woman. This is isolation from patients or vaccination before pregnancy from measles, rubella, chicken pox, influenza and ARVI; fencing from communication with patients and carriers of cytomegalovirus infection, other childhood infections. Viruses for pregnant women are especially dangerous, since they release toxins that depress the bone marrow, resulting in a decrease in platelet production and thrombocytopenia.
Also, when confirming pregnancy, you must refuse to vaccinate and take certain medications, namely:
- antineoplastic;
- aspirin;
- other anticoagulants and antiaggregants.
Also it is necessary to be protected as much as possible from the effects of chemical toxins, irradiation.
It is necessary to eat all the necessary vitamins, nutritional supplements, which will have a positive effect on the state of the immune system and the health of the fetus. Also in the early stages of pregnancy, a consultation of the hematologist and genetics is shown, especially if cases of thrombocytopenia of a hereditary character are recorded in the family.
Risks For The Neonate And Management
After delivery, close monitoring of the neonate is required as 21% to 28% will develop thrombocytopenia presumably from passive transfer of maternal autoantibodies against platelet antigens . The majority have mild thrombocytopenia without life threatening bleeding. Less than 1% of neonates develop intracranial hemorrhage . Risk for thrombocytopenia is increased if siblings had thrombocytopenia at delivery or if the mother has had a splenectomy . Except for one retrospective case series , most data suggest the mothers treatment and platelet counts during pregnancy do not impact the risk of thrombocytopenia in the neonate . Attempts to measure the fetal platelet count by percutaneous umbilical blood sampling is not recommended as there is a risk of hemorrhage and fetal loss comparable to non-intervention . Fetal scalp vein sampling also has a risk of hemorrhage and may result in a falsely low platelet count.
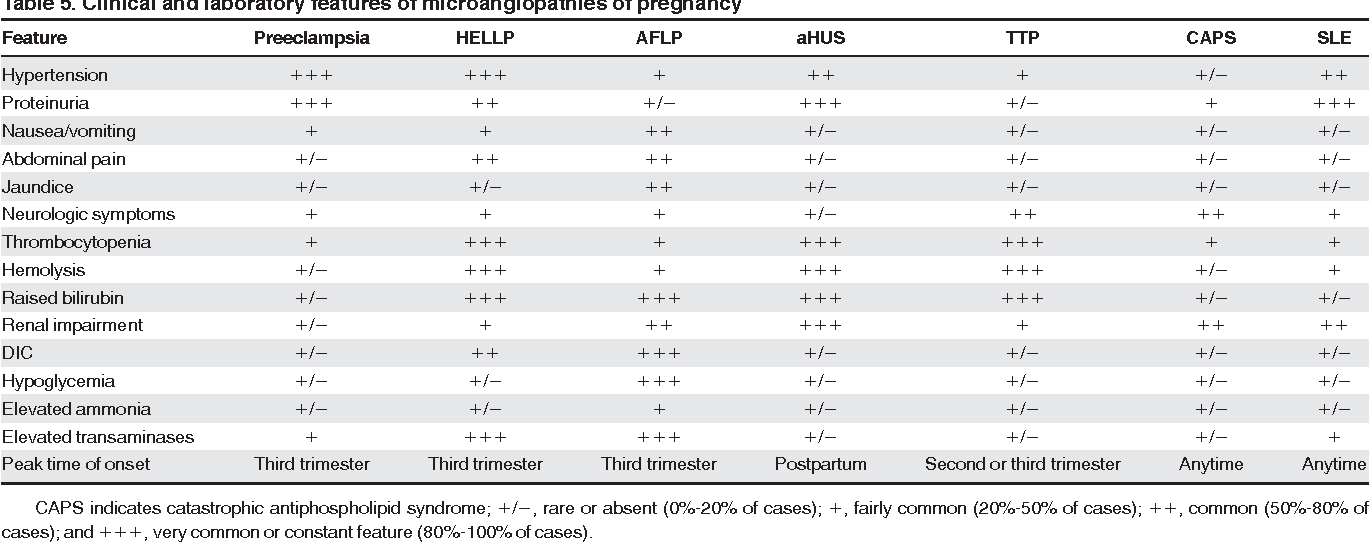
What Is The Standard Management Of Thrombotic Microangiopathies Of Pregnancy
The mainstay of treatment of preeclampsia/eclampsia, HELLP syndrome, and AFLP is delivery of the fetus.; Sudden deterioration in maternal and fetal conditions is common in pregnancies complicated by these disorders. Prompt delivery is indicated for pregnancies 34 weeks of gestation, evidence of fetal distress , or severe maternal disease . For pregnancies of < 34 weeks’ gestation and in which the maternal and fetal status is reassuring, glucocorticoids are recommended to accelerate fetal pulmonary maturity followed by delivery within 48 hours. Reversal of coagulopathy may be required before delivery and/or in the immediate postnatal period. The target platelet count for safe cesarean delivery is conventionally set at > 50 × 109/L, and this is the threshold we use in our practice. We consider expectant management performed under close maternal and fetal surveillance, only in selected cases for no more than 48-72 hours and only in patients < 34 weeks of gestation. It is understood that, if maternal conditions deteriorate, cesarean delivery should be performed immediately. The presence of DIC is considered a contraindication to conservative treatment.
Suggested approach to the management of patients with HELLP syndrome. EGA indicates estimated gestational age.
Recommended Reading: How Soon Can You Get Pregnant After Your Period Ends
What Testing Should Be Ordered When A Patient Presents With Thrombocytopenia During Pregnancy
reports the set of laboratory tests we use in our investigation of pregnant patients with thrombocytopenia. A careful review of the peripheral blood smear remains the main diagnostic procedure. shows our algorithm for workup of thrombocytopenia based on the observation of the peripheral blood film. Screening for coagulation abnormalities , liver function tests , antiphospholipid antibodies and lupus anticoagulant, and serologies for systemic lupus erythematosus are done if laboratory data, history, and physical examination suggest the thrombocytopenia may be secondary. Viral screening and Helicobacter pylori testing are recommended. Abnormalities of thyroid function are not uncommon in both ITP and pregnancy and associated with significant pregnancy-related complications and fetal risk,; and we do this testing routinely. If the past medical history suggests frequent infections, quantitative immunoglobulin testing may be appropriate.; If available, review of preexisting laboratory data may reveal abnormalities that preceded the pregnancy or were present only during a prior pregnancy.
Type 2b Von Willebrand Disease

This is a rare subtype of VWD, with increased affinity for platelet receptor glycoprotein 1b, which binds to platelets inducing spontaneous platelet aggregation, accelerating platelet clearance and hence causing thrombocytopenia.
During pregnancy, the abnormal VWF increases and thrombocytopenia may become evident or more pronounced, with the platelet count occasionally falling as low as 20â30 Ã 109/l. Women with type 2B VWD should be managed by a multidisciplinary team at a haemophilia centre. There is variability of response of VWD to pregnancy, and regular monitoring of the VWF, factor VIII level, and platelet count is essential. These should be taken at booking, before invasive procedures, and at 28 and 34 weeks.
Don’t Miss: How Soon Should You See An Obgyn When Pregnant
Immune Changes In Pregnancy
Pregnancy induced immunomodulation undoubtedly impacts ITP and new onset ITP during pregnancy likely represents a form of secondary ITP. Complex immune changes occur both systemically and at the maternal fetal interface at the placenta, allowing the maternal immune system to tolerate paternal alloantigens. Reduced exposure to paternal human leukocyte antigens may be critical for tolerance; fetal extravillous trophoblasts that migrate into the decidual lack expression of classical HLA class Ia and class II molecules and instead have non classical HLA class Ib molecules . Maternal tolerance is also regulated by hormones such as increased progesterone and beta HCG, which promote maternal immune cells to shift from an inflammatory to regulatory cytokine profile . While immunomodulation of pregnancy promotes tolerance of the fetus, the maternal immune system is not functionally immunosuppressed and may be more responsive to systemic infections . More research is needed to clarify how the immune changes of pregnancy alter autoimmunity.
Main Symptoms And Dangers
Symptoms of thrombocytopenia in pregnant women are somewhat more diverse than those in regular patients. Symptoms in women:
- bruises caused by touching, sometimes they are formed without external influences;
- bleeding nose and gums, but the latter is not always specific, since gingivitis pregnant develops in many women without deficiency of platelets in gestation period;
- gastro-intestinal bleeding, including hemorrhoids and fissure;
- dotty hemorrhages on the limbs and anterior surface of the trunk;
- vaginal bleeding.
Untreated thrombocytopenia can lead to serious complications of the pregnancy and delivery process. The most dangerous is massive bleeding, which can result in patients death. In addition, during the autoimmune process, antibodies penetrate the placenta into the bloodstream of the fetus. In this case, the newborn may develop thrombocytopenia.
Also Check: Can You Have Postpartum Depression During Pregnancy
Diagnosis And Differential Diagnosis
Pregnancy-related versus nonpregnancy-related
Causes of thrombocytopenia may be specific complications of pregnancy, be associated with an increased frequency in pregnancy, or have no relationship to pregnancy.
Pregnancy-specific complications
Gestational thrombocytopenia, also known as incidental thrombocytopenia of pregnancy, is the commonest cause of thrombocytopenia in pregnancy occurring in approximately 75% of cases. It is a diagnosis of exclusion, no confirmatory tests are available. It generally causes mild thrombocytopenia with the majority of cases having platelet counts of 130 to 150 x 109/L. Most experts consider this diagnosis unlikely if the platelet count falls below 70 x 109/L.
It occurs in the middle of the second trimester and the third trimester and is not associated with maternal bleeding. During pregnancy, it is not possible to differentiate between the more severe form of gestational thrombocytopenia and primary immune thrombocytopenia as both are diagnoses of exclusion. For the thrombocytopenia to be consistent with gestational thrombocytopenia, women should have no history of thrombocytopenia , the thrombocytopenia should resolve spontaneously within 1 to 2 months in all cases and the fetus/neonate should not be affected by thrombocytopenia.
Pregnancy-associated conditions
Nonpregnancy associated
Viral infection
Diagnostic approach
ITP
>30 x 109/L â no treatment required in 1st and 2nd trimesters
>50 x 109/L â procedures safe
Treatment
TTP/HUS
What Is The Risk To The Neonate How Should He Be Monitored
Platelet counts < 50 × 109/L occur in 10% of newborns of mothers with ITP, whereas platelet counts < 20 × 109/L occur in 5% of cases.; Intracranial hemorrhage has been reported in 0%-1.5%.,,; There are no indirect ways of measuring the fetal platelet count, and the correlation between maternal and fetal platelet counts is poor.,; The best predictor of severe thrombocytopenia at birth is its occurrence in an older sibling,,,; Maternal response to treatment does not automatically protect the newborn from the development of thrombocytopenia. On the other hand, there is no robust evidence to suggest that neonates from women with ITP poorly responsive or refractory to treatment have a higher risk of severe thrombocytopenia.
Don’t Miss: When Can You Find Out You Are Pregnant
What Are The Reasons For Platelets Count Lowering In Pregnancy
Thrombocytopenia or critical reduction of platelets in the blood analysis can be caused by several factors:
- AIDS;
- Leukemia;
- Lupus.
However, Thrombocytopenia in pregnancy may occur without these reasons and, as a rule, this does not lead to any serious complications. Standard techniques used to increase the number of platelets in the blood may vary depending on the case severity.
Very low platelets count in the analysis is can indicate at unstoppable bleeding in a patient, this is the threshold beyond which Thrombocytopenia is transformed into a real problem. In this case, if the platelet count drops below 100,000 units per µL, the medical staff of maternity hospitals normally refuses to provide an epidural or a cesarean section.
In fact, a non-critical level of platelets in pregnancy can be caused by trivial malnutrition or improper diet of the future mother. The following guidelines are to help pregnant tackle this problem.
How Should Delivery Be Managed What Is A Safe Platelet Count For Epidural Anesthesia
ITP is not an indication for cesarean delivery.,; Mode of delivery in a pregnant patient with ITP is based on obstetric indications, with avoidance of procedures associated with increased hemorrhagic risk to the fetus .; Most neonatal hemorrhages occur at 24-48 hours and are actually not related to trauma at the time of delivery.,; Determination of the fetal platelet count by fetal scalp vein blood draws or periumbilical blood sampling presents a potential hemorrhagic risk to the fetus and may inaccurately predict a low platelet count.; For this reason, fetal platelet count measurement is not recommended.
Maternal anesthesia must be based on safety of the mother. The precise platelet count needed to safely perform neuraxial analgesia is unknown.,; American guidelines do not suggest any particular threshold but individual assessment of risks and benefits.; Local practices may actually differ significantly. Our anesthesiologists will generally withhold spinal anesthesia for women with platelet counts < 80 × 109/L. For patients who have not required therapy during gestation but have platelet counts below this threshold, we administer short-term corticosteroids for 1-2 weeks or IVIg to raise the platelet count for the procedure. Platelet transfusion is not appropriate to prepare for spinal anesthesia; post-transfusion increments may be inadequate or short-lived and should be reserved to treat bleeding.
You May Like: What To Know At 6 Weeks Pregnant
Itp Patients With Moderate/severe Thrombocytopenia
The usual first-line treatment is prednisolone, but at much lower doses than used out with pregnancy, 10â20 mg daily for a week, adjusting to the minimum dose that achieves a haemostatically effective platelet count . Response time is as for non-pregnant women, 3â7 d, as is response rate. Maternal risks include inducing or exacerbating gestational diabetes, maternal hypertension, osteoporosis, weight gain, and psychosis. Platelet count may fall more rapidly near term, so defer dose adjustment until after delivery, and then taper slowly to avoid a rapid fall in platelet count and to ensure the mother’s psychological state is not affected.
In the short term, low-dose steroids are considered safe and effective for the mother. However, low dose maternal steroids do not have any beneficial effect on the fetal platelet count . Prednisolone is metabolized by the placenta but high doses have the potential to cause effects on the fetus including premature rupture of membranes, adrenal suppression, and a small increase in cleft lip after use in the first trimester .
What Causes Thrombocytopenia
The most common causes of thrombocytopenia are lab error , gestational thrombocytopenia, preeclampsia, and autoimmune thrombocytopenia, including idiopathic thrombocytopenic purpura . Other rare causes of thrombocytopenia are disseminated intravascular coagulation , thrombotic thrombocytopenic purpura and hemolytic-uremic syndrome , congenital platelet disorders, bone marrow disease, and hypersplenism .
Don’t Miss: How Yk If You Pregnant
Low Platelets And Pregnancy
Primary immune thrombocytopenia targets platelets, marks them as foreign by the immune system causing them to be eliminated in the spleen and sometimes, the liver. ITP is defined by a platelet count lower than 100,000 per microliter of blood with no other reason for low platelets.
Interestingly, low platelet counts are a normal part of pregnancyeven for those without a primary ITP diagnosis. In fact, thrombocytopenia is often discovered during pregnancy and has been observed in seven to 10 percent of all pregnancies.
In uncomplicated pregnancies, the platelet count will often drop about 10 percent. For most women this drop in platelets does not result in thrombocytopenia. But if a woman were at the low end of the normal range, such as 160,000 platelets per microliter, and her platelets drop 10 percent to 144,000 per microliter, she would become thrombocytopenic. Even if there werent a history of thrombocytopenia or other medical problems, she would be considered to have gestational thrombocytopenia , which occurs in five to eight percent of healthy women
Yet, it is important to determine if the low platelet count is gestational thrombocytopenia or due to another cause, such as ITP. Research has helped define ways to tell if low platelets in pregnancy are due to ITP or some other cause and the best way to treat the condition.
What Is The Most Probable Etiology Of Her Thrombocytopenia
Preeclampsia is the second most frequent cause of thrombocytopenia developing in the late second or third trimester, accounting for 21% of cases of thrombocytopenia at the time of delivery.; It is defined by new onset hypertension with 140 mmHg systolic or 90 mmHg diastolic blood pressure after 20 weeks’ gestation together with proteinuria .; Approximately 15%-25% of women with gestational hypertension will develop preeclampsia.; In some women, the signs of preeclampsia can present as late as 4-6 weeks postpartum. There are very few data on the proportion of preeclampsia that occurs antepartum versus postpartum, but reports of the incidence of new-onset postpartum hypertension or preeclampsia range from 0.3% to 27.5%.; The diagnosis of eclampsia is made with the onset of seizures that cannot be attributed to other causes in a woman with preeclampsia.
Thrombocytopenia may be the only initial manifestation of preeclampsia. Platelet counts < 50 × 109/L occur in < 5% of preeclamptic women.; Intravascular hemolysis resulting from red cell fragmentation can accompany severe preeclampsia but is usually not a prominent feature. Coagulation abnormalities are unlikely if the count is > 100 × 109/L.; Transaminases and LDH levels may be elevated, although less than seen in the HELLP syndrome.
Recommended Reading: Can You Get Lasik Eye Surgery While Pregnant
What Causes Low Platelets In Pregnancy
Outside of pregnancy, a normal platelet count ranges from 150,000 to 450,000/µL .
It’s normal for your platelet count to dip by a few thousand during pregnancy, due in part to hemodilution: the body makes more plasma during pregnancy, so the total number of platelets per volume of blood will be lower.
When the number dips below 100,000-150,000/µL, your doctor will want to keep a closer eye on you to reduce the risk of complications.
During pregnancy, about 10 percent of women have platelets counts below 150,000/µL. Of these, approximately:
- 75 percent are due to normal changes in pregnancy
- 21 percent are related to hypertensive diseases, such as preeclampsia or HELLP syndrome
- 4 percent are due to inherited or immunological conditions in which the immune system makes antibodies which attack platelet cells
Approximately 1 percent of patients have platelets counts of less than 100,000/µL, which might impact pregnancy management.
Platelets may be destroyed at a higher rate in pregnancy. As the spleen increases in size due to increased blood volume during pregnancy, it may destroy more platelets in the filtering process.
A severe lack of folic acid in your blood can cause thrombocytopenia, so it is important to take your prenatal vitamins. Certain bacterial and viral illnesses such as Epstein-Barr, HIV, and hepatitis B and C can also lower your platelet count.
Management Of Ttp In Pregnancy
Any delay in treatment for TTP is life-threatening for mother and baby; treatment with PEX should be commenced without delay. Regular PEX may enable pregnancy to continue successfully . The optimal frequency of PEX during pregnancy is unknown. Where possible, delivery is the treatment of choice for pregnancy-associated microangiopathies, however delivery does not guarantee remission .
You May Like: How To Get Fit While Pregnant
Is It Possible To Prevent Gestational Thrombocytopenia
No, gestational thrombocytopenia is simply an exaggeration of the normal drop in platelets that occurs with pregnancy. Women who have gestational thrombocytopenia with one pregnancy are more likely to have it with subsequent pregnancies, but the condition is also benign with these subsequent pregnancies.

