Discount Medical Plan Organization
If negotiating your own self-pay discount scares you, you can work with a Discount Medical Plan Organization. These companies provide pre-negotiated discounts to their members for a monthly fee.
This isnt true maternity insurance since youre paying the doctor and hospital yourself, but the discount has already been negotiated for you by the DMPO.
Before you enroll, make sure your doctor and hospital participate, as many plans have a severely limited selection of participating healthcare providers. If you havent yet selected a doctor or hospital, however, you can limit your selections to providers who participate in the DMPO.
Also Check: Can You Have Lasik While Pregnant
Can A School Make A Pregnant Or Parenting Student Take Different Classes Or Quit Activities
Students who are pregnant, or who have become parents before turning 18, may wonder if their school make them take different classes, or make them quit extracurricular activities or sports.
The federal law known as Title IX is the main law that protects a student who becomes pregnant or is a parent. 20 U.S.C. sections 1681 through 1688. This law prevents a school from discriminating against a student in all academic, educational, extracurricular, athletic and other programs or activities available to students in the school district. This includes protecting against discrimination based on pregnancy or conditions related to pregnancy, such as childbirth, termination of pregnancy, or recovery from birth or termination of a pregnancy.
This means that a school district cannot exclude you from any activities because you are pregnant, experiencing a condition related to pregnancy, or are a parent, regardless of your gender.
While a school district can provide students like you with special programs or classes, these classes and programs must be similar to the other classes offered to all students, and your decision to attend a special program or class must be completely voluntary.
Can A Pregnant Woman Receive Medicaid Or Chip Services Prior To An Eligibility Decision
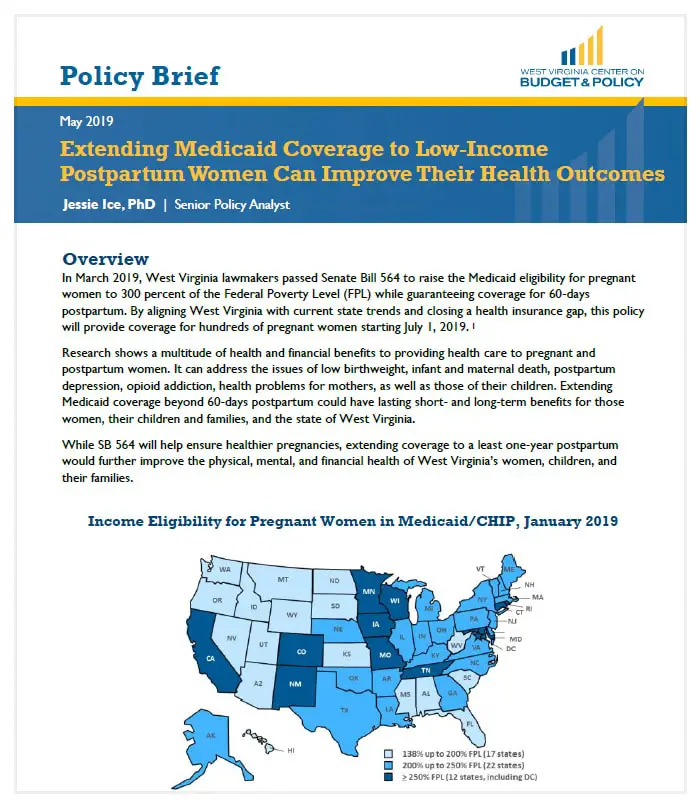
Maybe. States may elect, but are not required, to provide some categories of Medicaid enrollees, including pregnant women, with presumptive eligibility. This allows pregnant women to receive immediate, same-day Medicaid services, typically at the clinic or hospital where they submit an application for Medicaid presumptive eligibility. Currently, 30 states provide presumptive eligibility to pregnant women.
Don’t Miss: How To Know If Your Pregnant
If You Have Medicaid Or Chip
- If found eligible during your pregnancy, youll be covered for 60 days after you give birth. After 60 days, you may no longer qualify. Your state Medicaid or CHIP agency will notify you if your coverage is ending. You can enroll in a Marketplace plan during this time to avoid a break in coverage.
- If you have Medicaid when you give birth, your newborn is automatically enrolled in Medicaid coverage, and theyll remain eligible for at least a year.
Also Check: Can You Donate Plasma When Pregnant
How Much Does It Cost To Have A Baby With No Insurance
You should make sure you are well-prepared financially for this part of pregnancy, especially if you dont have health insurance. The costs of childbirth can be steep. The charge for an uncomplicated cesarean section was about $15,800 in 2008. An uncomplicated vaginal birth cost about $9,600, government data show.
Recommended Reading: Can I Put Braces While Pregnant
If You May Qualify For Medicaid Or The Childrens Health Insurance Program
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
How To Apply For Medicaid Online In Texas
You can apply for Medicaid online in TX through the health exchange. Once you are there, you need to create a unique username and password to access data for your region. Then, you will be asked a series of questions. Note that all Medicaid application methods require specific documents and/or information to be transmitted to the states health department.
Certain items are non-negotiable when it comes to completing Texas Medicaid application forms. Whether you are filing a Medicaid online application or not, you must have the following handy:
- Your Social Security Number
- Information on any assets you have acquired
- The size of your household
If your TX application for Medicaid is on behalf of your family, you must also provide all of the above information for each member. To make sure you are fully prepared for the application process, .
If you already have health insurance, you will have to answer questions about your current medical coverage. You may still be able to qualify for Medicaid depending on your circumstances.
People with disabilities and minors have eligibility for TX healthcare benefits. If you have a disability, be sure to mention it on your Texas Medicaid application forms . Finally, you will be asked to verify all the information you have entered and to sign your application for Medicaid electronically.
Donât Miss: Can You Get Lasik Eye Surgery While Pregnant
Read Also: What Happens If I Get Nexplanon While Pregnant
Do Medicaid And Chip Provide Pregnant Women With Comprehensive Health Coverage
Yes, in most but not all states. Full-scope Medicaid in every state provides comprehensive coverage, including prenatal care, labor and delivery, and any other medically necessary services.
Pregnancy-related Medicaid covers services necessary for the health of a pregnant woman and fetus, or that have become necessary as a result of the woman having been pregnant. Federal guidance from the Department of Health and Human Services clarified that the scope of covered services must be comprehensive because the womans health is intertwined with the fetus health, so it is difficult to determine which services are pregnancy-related. Federal statute requires coverage of prenatal care, delivery, postpartum care, and family planning, as well as services for conditions that may threaten carrying the fetus to full term or the fetus safe delivery. The state ultimately decides what broad set of services are covered. Forty-seven states provide pregnancy-related Medicaid that meets minimum essential coverage and thus is considered comprehensive. Pregnancy-related Medicaid in Arkansas, Idaho, and South Dakota does not meet MEC and is not comprehensive.
CHIP coverage for pregnant woman is also typically comprehensive. However, in states where services are being provided to the pregnant woman by covering the fetus, the services may not be comprehensive with respect to the health needs of the pregnant woman.
Can An Uninsured Woman Enroll In Marketplace Coverage Upon Giving Birth
Maybe. If the baby is eligible for Marketplace coverage, then the baby qualifies for an SEP as a new dependent. In such instances, the regulations will also permit an SEP for the new mother, as someone who has gained a dependent through birth.
WOMEN ALREADY ENROLLED IN FULL-SCOPE OR EXPANSION MEDICAID
Don’t Miss: How You Know If You Pregnant
What Is Included In The Birth Baby And Beyond Program
Our program helps pregnant CCP members with everything from finding a doctor to birth planning to baby supplies and more. We will connect you with local experts in Broward County for prenatal and postpartum care
Our Birth, Baby, and Beyond program includes more than just health care coverage. We help mothers with many services before, during, and after pregnancy.
If you are a CCP Medicaid member, call us at 1-866-899-4828 for help with:
- Finding a doctor for you and your baby
- Making early prenatal and postpartum care appointments
- Educational facts and information about your babyâs care, safety and breastfeeding
- Getting transportation
- Baby supplies, food, prenatal classes, housing, and breastfeeding assistance
- Making delivery plans
If you would like a team member or nurse to contact you, please fill out ouremail form.
Our team of trained Obstetrics nurses will be your guides to every important health step for you and your baby. This includes checking for any health risks to give and your baby the right level of care. You can also trust our team for friendly appointment reminders, helpful tips, or even just a good listener when you need one.
For more information, you can view or download our.
If you do not speak English: Please call us at . We can help answer your questions in your language. We can also help you find a health care provider for your language.
Mothers Find Their Own Stopgaps In The Face Of Crisis
The urgent need to fix the gaps in postpartum care has captured the attention of national reformers, who see it as a critical step toward narrowing racial disparities in maternal mortality. Several 2020 Democratic presidential candidates have proposed federal legislation to extend pregnancy Medicaid to a full year postpartum, and state lawmakers have introduced a wave of similar bills. Missouri passed a limited extension last year and Illinois a far more sweeping one this past July both plans are awaiting federal approval.
The enthusiasm extended to Texas, where a broad coalition, led by the maternal mortality review task force, came together this past legislative session to support a full-year extension. The effort passed the House but stalled in the Senate. All the oxygen in the room this session was taken up by school finance reform, the legislative priority of the states top Republicans, said Tim Schauer, an Austin-based lobbyist on womens health issues.
The five-year cost of extending postpartum coverage was estimated at nearly $1 billion in state and federal funds, according to Politico. Rep. Shawn Thierry , who introduced one of the extension bills, had to counter skeptics who thought that the states alarming maternal mortality numbers were, as she said, kind of a hoax and that increasing benefits for new mothers was just a stealth tactic aimed at expanding Medicaid more widely.
Read Also: Is Vagisil Safe To Use While Pregnant
Also Check: How To Get Pregnant After Birth Control Shot
Medicaid Eligibility For Adults
Adults may be eligible if you:
- are a Virginia resident, age 19 to 64
- are a United States citizen or lawfully-residing immigrant
- are not eligible or covered by Medicare
- you are medically complex
- meet the income requirements based on your household size.
You are eligible for the Commonwealth Coordinated Care Plus program when you have full Medicaid benefits and meet one of the following conditions:
- you are a Virginia resident, age 65 and older
- you are an adult or child with a disability
- you reside in a nursing facility
- you receive services through the CCC Plus home and community-based services waiver
- or you receive services through any of the three waivers serving people with developmental disabilities , also known as the DD Waivers
If You Dont Have Health Coverage
- Health coverage makes it easier to get the medical check-ups and screening tests to help keep both you and your baby healthy during pregnancy.
- If you qualify for a Special Enrollment Period
A time outside the yearly Open Enrollment Period when you can sign up for health insurance. You qualify for a Special Enrollment Period if youâve had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
due to a life event like moving or losing other coverage, you may be able to enroll in a Marketplace health plan right now. Being pregnant doesnât make you eligible, but the birth of a child does.
- Create an account now to apply for Marketplace coverage through the Open Enrollment Period or a Special Enrollment Period. If you select the option to get help paying for coverage on your application, youâll be asked if youâre pregnant. Reporting your pregnancy may help you and your family members get the most affordable coverage.
- If you donât qualify for a Special Enrollment Period right now, you� âll be eligible to apply within 60 days of your childâs birth. You can also enroll in coverage for the next plan year during the next Open Enrollment Period this fall.
- If eligible for Medicaid or CHIP, your coverage can begin at any time.
You May Like: How Often Can Precum Cause Pregnancy
What Happens After I Apply For Medicaid In Florida
After you submit your Florida Medicaid application, you may be required to attend an interview with a Department of Children & Families case worker.
Whether you will required to attend an interview depends on your situation:
If you are applying for Medicaid for your child alone, then no interview will likely be required.If you are applying for any other benefits at the same time, then an interview will likely be required.
During this interview, you will be required to bring documents that prove the information that you provided on your initial Florida Medicaid application.
See above for the list of documents that may be required during the interview.
Once you complete this interview, you will receive a call or a letter in the mail that will tell you whether you were approved or denied.
If you are denied benefits, you have the right to appeal but that appeal must be filed within a certain timeframe. As your caseworker for details.
Recommended Reading: Pregnancy Medicaid Florida Phone Number
Medicaid Coverage And State
Private health insurance covers the cost of substance-use disorder treatment and services to varying degrees. Each insurer has its own policy, and insured individuals will need to refer to the policy of their respective insurance companies to determine the extent of services that are covered. Many women needing treatment, including pregnant women, may have once had private insurance but have lost that insurance. This section presents information for women who are uninsured, women who may qualify for Medicaid insurance, and women who are currently insured with Medicaid.
Medicaid Services for Women and Children
- Medicaid for Infants and Children
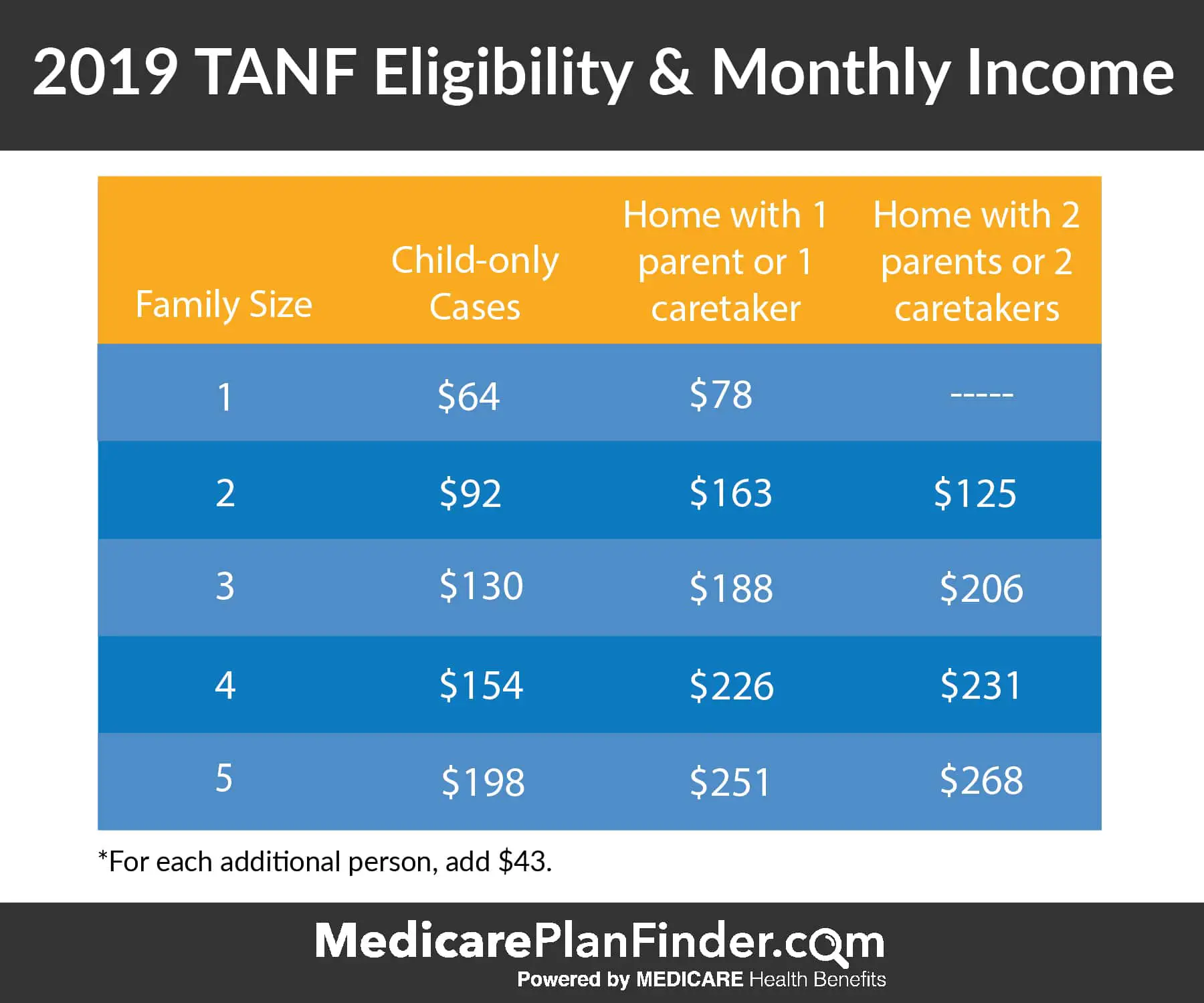
Medicaid for Infants and Children provides medical coverage for children younger than 19 years old. The income limits are determined by the family size and the age of the child or children applying for benefits. There is no limit on resources.
- Medicaid for Families with Dependent Children
Medicaid for Families with Dependent Children provides medical coverage for parent or other caretaker/relative with a child 18 years or younger in the household and for children under age 21. A pregnant woman may also qualify.
The family cannot have more than $3,000 in assets such as savings in the bank.
If the family income is above the cut-off and the child and/or family has high medical bills, the family might still qualify for Medicaid .
- Medicaid for Pregnant Women
Medicaid for Pregnant Women covers only services related to pregnancy:
Recommended Reading: How To Use Pills Not To Get Pregnant
Duration Of Medicaid Coverage
- Presumptive Eligibility for Pregnant Women
- Begins the date of application and lasts until DCF makes a determination of ongoing eligibility, or 60 days .
- Simplified Eligibility for Pregnant Women
- Begins the first day of the application month and lasts through two post-partum months. Lasts up to three months retroactive coverage available, if eligible and requested, provided woman was pregnant during the retroactive period.
- Other Medicaid, including Medically Needy
- Other Medicaid: Begins the first day of the application month and lasts through two post-partum months.
- Medically Needy: Begins the date that Share of Cost is met.
- Up to three months retroactive coverage available, if eligible and requested.
Im Pregnant Afraid Of My Parents And Staying With An Adult Whos Not My Parent Will They Get In Trouble
Minors may be in situations where they move in with another adult because they fear what their parents will do if they find out about a pregnancy . This raises the question of whether the adult the minor is staying with could be arrested.
If you are not legally emancipated and you reside with another adult without your parents permission, then they could be arrested for kidnapping or interfering with child custody or possession.
Recommended Reading: How To Treat Uti In Pregnancy
Who Can Get Medicaid
- No matter your state, you may qualify for Medicaid based on your income, household size, disability, family status, and other factors. But if your state has expanded Medicaid coverage, you can qualify based on your income alone.
- Enter your household size and state. Well tell you who is eligible for Medicaid, if your state expanded and if you qualify for Medicaid based only on your income.
- If you think you have Medicaid eligibility, you can create an account and fill out a Marketplace application. If it looks like anyone in your household qualifies for Medicaid or CHIP, well send your information to your state agency. Theyll contact you about enrollment. You can apply any time of year.
- If you dont qualify for Medicaid, well tell you if you qualify for financial help to buy a Marketplace health plan instead.
Where To Submit Your Medicaid Application
You can submit your application in the following ways.
- Mail The PO Box is found on the 1st page of the Medicaid application.
- Fax You can also find the fax number on the 1st page of the application.
- In-person Refer to the section below to find a Houston Medicaid office, call 211 or visit Your Texas Benefits.
- Online If you change your mind and want to complete the Medicaid application online, visit Your Texas Benefits.
- Phone You also call 877.541.7905 to apply for Medicaid.
Note: If you do not feel safe visiting a Medicaid office due to COVID 19, consider applying by mail or online.
Read Also: How To Prevent Stretch Marks While Pregnant

