How Is Group B Strep Diagnosed
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be “GBS positive.” This means only that she has the bacteria in her body not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
When To Undergo The Group B Strep Test
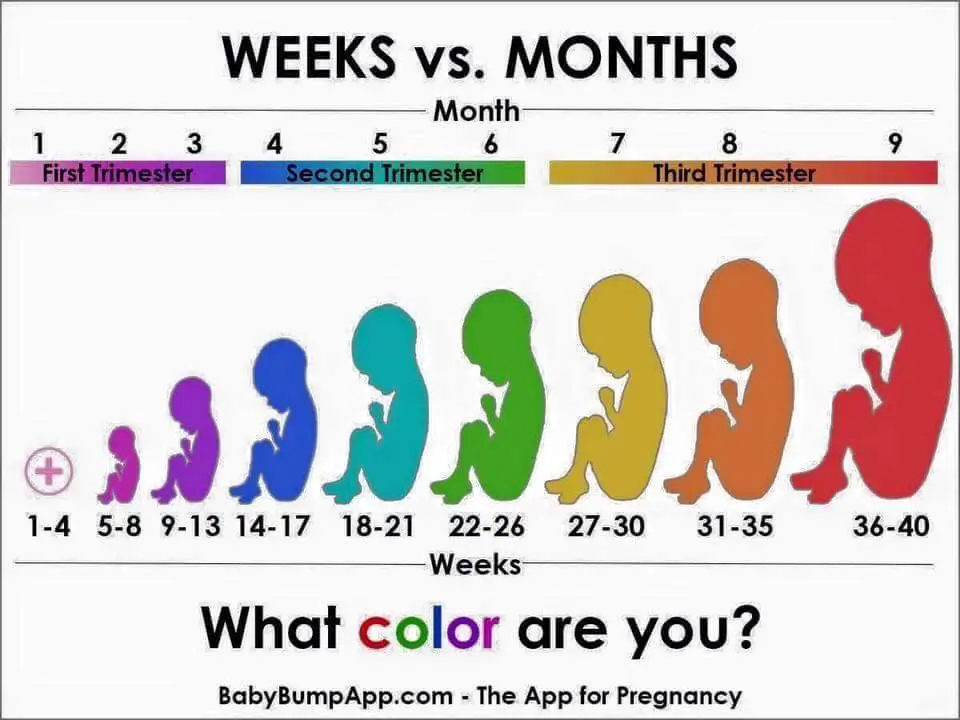
Health care providers usually perform group B strep tests during the third trimester, specifically between the 36th and 37th weeks of pregnancy. By testing in the weeks leading up to the birth, your health care providers ensure they have up-to-date information when you go into labor.
The strep B test is a relatively simple procedure, and it doesnt require any preparation. If this isnt your first pregnancy, make sure to inform your health care provider about your previous group B strep results. Let them know whether you tested positive or negative for the bacteria and whether your baby was affected by it.
Gbs During Pregnancy: Risks And Complications
Its important to know that even if you have GBS during pregnancy, your baby will probably be healthy.
Even if mama has Group B Strep and is NOT treated, there is only a 1-2 percent chance that baby will get an infection. Antibiotics during labor further decrease the risk to about 0.2 percent.
That said, GBS should be taken seriously, because infections can be life-threatening for baby. If baby contracts an infection from GBS, it is usually treatable, but it can be serious and very scary. Complications range from fever to more critical issues, such as pneumonia, sepsis, and meningitis . In 2-3 percent of full-term babies, a GBS infection is fatal.
You May Like: Is It Safe To Use Vagisil While Pregnant
How Common Is Gbs
- GBS is carried in the vagina and bowel of about 3 in 10 women in the UK.
- GBS is the most common cause of severe infection in newborn babies. It is the most common cause of meningitis in babies under the age of 3 months.
- On average in the UK, about 1 in 2,000 newborn babies are diagnosed with early-onset GBS infection.
How Can We Reduce The Risk Of My Baby Developing Gbs Infection
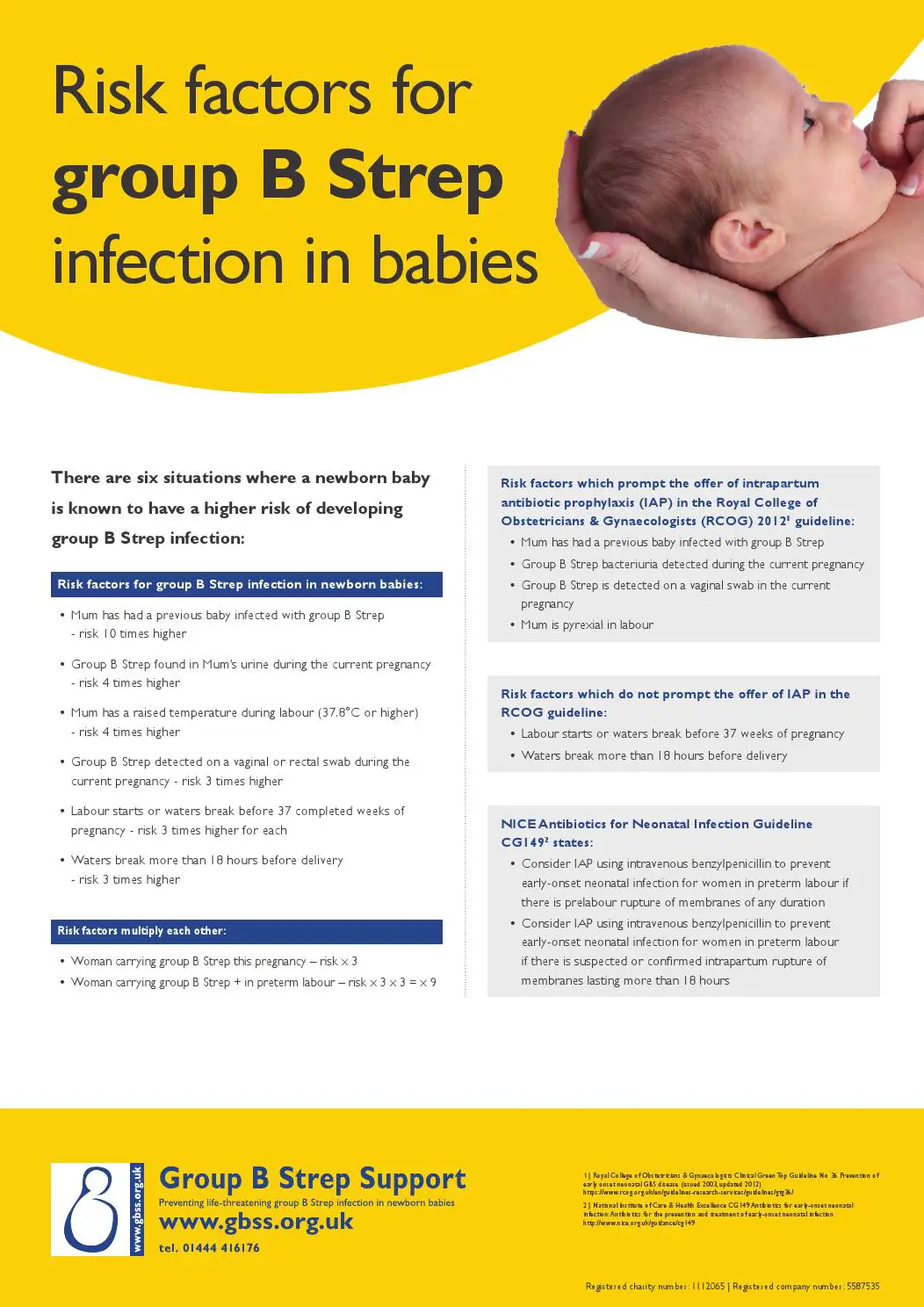
Depending on your circumstances, you may be offered antibiotics through a drip from the start of labour and at intervals until your baby is born. You wont be offered antibiotics before labour because this does not reduce the chance of your baby developing GBS infection.
These antibiotics reduce the risk of your baby developing a GBS infection in their first week of life from around 1 in 400 to 1 in 4,000. Your healthcare professional should talk to you about the benefits and risks of taking these antibiotics.
Recommended Reading: Safe To Take Tums While Pregnant
Can Baby Get Gbs During A C
If you are GBS positive and your water breaks, baby can be colonized with Group B Strepregardless of whether you end up having a vaginal birth or a C-section. This is because the physical barrier protecting baby, aka the bag of waters, has been compromised. The longer baby remains inside the mother after her water breaks, the higher the risk of infection .
Group B Strep And Pregnancy
Group B Streptococcus is a type of bacteria which lives in the intestines, rectum and vagina of around 2-4 in every 10 women in the UK . This is often referred to as carrying or being colonised with GBS.
Group B Strep is not a sexually transmitted disease. Most women carrying GBS will have no symptoms. Carrying GBS is not harmful to you, but it can affect your baby around the time of birth.
GBS can occasionally cause serious infection in young babies and, very rarely, during pregnancy before labour.
Also Check: Lice Shampoo And Pregnancy
Discussing Group B Streptococcus
Discussion about Group B streptococcus should take place at around 35 weeks gestation so that women have received information about preventive treatment before they go into labour. This timing also enables testing at 3537 weeks and receipt of test results, if testing is being offered. Points for discussion include:
- Group B streptococcus is part of the normal bacteria that live in the body and anyone can become colonised with Group B streptococcus without having symptoms
- Group B streptococcus is transmitted to the baby during the birth in 12 per 1,000 live births and can cause serious infection in the newborn
- treatment with intravenous antibiotics during labour reduces the risk of transmission of the infection to the baby
- women may be advised to remain in hospital for at least 24 hours after the birth so that the baby can be observed for signs of Group B streptococcus infection.
Frequently Asked Questionsexpand All
- What is group B streptococcus?
Group B streptococcus is one of the many bacteria that live in the body. It usually does not cause serious illness, and it is not a sexually transmitted infection . Also, although the names are similar, GBS is different from group A streptococcus, the bacteria that causes strep throat.
- Why is group B streptococcus a concern for pregnant women?
In women, GBS most often is found in the vagina and rectum. This means that GBS can pass from a pregnant woman to her fetus during labor. This is rare and happens to 1 or 2 babies out of 100 when the mother does not receive treatment with antibiotics during labor. The chance of a newborn getting sick is much lower when the mother receives treatment.
- How can group B streptococcus affect a newborn?
Even though it is rare for a baby to get GBS, it can be very serious when it happens. Babies who get GBS may have early-onset or late-onset disease.
- What is early-onset disease?
With early-onset disease, a baby typically gets sick within 12 to 48 hours after birth or up to the first 7 days. Early-onset disease can cause severe problems, such as
-
inflammation of the covering of the brain or spinal cord
-
infection of the lungs
-
infection in the blood
A small number of babies with early-onset disease die even with immediate treatment.
Lack of energy
High fever
You had a previous child who had GBS disease
You have GBS bacteria in your urine at any point during your pregnancy
Don’t Miss: Can You Get Lasik Eye Surgery While Pregnant
Gbs Hyaluronidase Impedes Immune Detection And Aids In Ascension To The Uterus
Hyaluronan levels increase in the cervix throughout pregnancy, reaching their height during parturition. This glycosaminoglycan plays a structural role in the ECM, and plays additional roles in cell migration, adhesion, and inflammation through its digestion into fragments that interact with a diverse array of host receptors, including toll-like receptor 2 and 4 . HA is crucial for maintaining epithelial polarization and barrier function, and loss of HA is associated with ascending infection and subsequent infection-induced PTB . Additionally, low molecular weight HA serves as a damage-associated molecular pattern that initiates TLR2 and 4-mediated inflammation during tissue injury . GBS exploits this axis through the secretion of hyaluronidase , which cleaves the pro-inflammatory HA DAMPs into disaccharides, which bind to TLR2/4 and block recognition of GBS ligands. This ultimately results in a dampened immune response . Interestingly, GBS clinical strains isolated from cases of PTB or invasive neonatal infection had high HylB activity, and HylB activity was associated with ascending infection, reduced uterine inflammation, and increased rates of PTB in mice . Although these studies partially define interactions in this immune evasion mechanism, the precise timing, immune mediators, and cell types involved remain unidentified.
What Does The Screening Test Involve
You will usually be screened for GBS between 35 and 37 weeks of gestation. The test is easy and painless, and is conducted by swabbing the vagina and rectum with a cotton-tipped swab. You have the option of doing the swabbing yourself. The swab is then cultured to see if GBS is present. Even if you have a planned Caesarean delivery, you will still need to be screened for GBS in case your water breaks or you go into labour before the scheduled delivery.
Don’t Miss: Is It Safe To Take Tums While Pregnant
What Happens During A Group B Strep Test
If you are pregnant, your health care provider may order a swab test or a urine test.
For a swab test, you will lie on your back on an exam table. Your health care provider will use asmall cotton swab to take a sample of cells and fluids from your vagina and rectum.
For a urine test, you will most likely be told to use the “clean catch method” to ensure your sample is sterile. It includes the following steps.
- Wash your hands.
- Clean your genital area with a cleansing pad given to you by your provider. To clean, open your labia and wipe from front to back.
- Start to urinate into the toilet.
- Move the collection container under your urine stream.
- Collect at least an ounce or two of urine into the container, which should have markings to indicate the amounts.
- Finish urinating into the toilet.
- Return the sample container as instructed by your health care provider.
If your baby needs testing, a provider may do a blood test or a spinal tap.
For a blood test, a health care professional will use a small needle to take a blood sample from your baby’s heel. After the needle is inserted, a small amount of blood will be collected into a test tube or vial. Your baby may feel a little sting when the needle goes in or out.
A spinal tap, also known as a lumbar puncture, is a test that collects and looks at spinal fluid, the clear liquid that surrounds the brain and spinal cord. During the procedure:
Symptoms Of Strep B In Adults
Most women do not show signs of carrying the GBS bacteria, so will only find out that they are carriers when theyre tested.
However, in some cases, GBS can cause the following symptoms in adults:
- Infections of the skin or soft tissue
- Infection of bone or joints
- Pneumonia
Related Article: Umbilical cord around neck symptoms, is it common and dangerous for the fetus?
You May Like: Can You Use Vagisil Wash While Pregnant
How Does Group B Strep Affect A Newborn Baby
Babies may experience early or late-onset of GBS.The signs and symptoms of early-onset GBS include:
- Signs and symptoms occurring within hours of delivery
- Sepsis, pneumonia, and meningitis, which are the most common complications
- Breathing problems
- Heart and blood pressure instability
- Gastrointestinal and kidney problems
Early-onset GBS occurs more frequently than late-onset. Intravenous antibiotics are used to treat mothers and newborns with early-onset GBS.The signs and symptoms of late-onset GBS include:
- Signs and symptoms occurring within a week or a few months of delivery
- Meningitis, which is the most common symptom
Late-onset GBS could have been passed during delivery, or the baby may have contracted it by coming in contact with someone who has GBS.
If You Have Group B Strep
If tests find group B strep, or you have had a baby that’s had it before, you may need extra care and treatment.
You may be advised to:
- review your birth plan with your midwife – the safest option may be to give birth in hospital
- contact the hospital as soon as your waters break or when you think you are in labour
- medically induce your labour if your waters break after 37 weeks. This will reduce the time your baby is exposed to group B strep before birth
- have antibiotics through a drip during the labour to reduce the chances of your baby becoming ill
- take a course of antibiotic tablets. This may be needed if group B strep is found in your urine and your GP or obstetrician thinks you have a urine infection
- stay in hospital for longer than planned so your baby can be monitored
Antibiotics used for group B strep are safe to take during pregnancy and birth. Always tell your prescribing doctor if you are allergic to any antibiotics.
You May Like: Can You Donate Plasma While Pregnant
What If You Test Positive For Group B Strep
There are health risks associated with strep B, but a positive test result only indicates the potential for infection. With proper treatment, you can minimize that risk, leading to a healthy outcome for you and your baby.
If you do test positive for group B strep, your health care provider will probably prescribe intravenous antibiotics during labor. There is no vaccine or pre-birth treatment you can take to protect against this bacteria. Because it is fast-growing and present in the birth canal, prescribing antibiotics before labor or by mouth isnt very effective.
To protect the baby from strep B exposure during labor, health care providers usually start pregnant women on a round of intravenous antibiotics about four hours before birth. This helps destroy any bacteria in the birth canal by the time the baby is born. When pregnant women test positive for group B strep bacteria, receiving antibiotics during labor can lower the risk of their baby developing GBS disease to 1 in 4,000.
During labor, babies can be exposed to group B strep when the amniotic sac breaks. If you plan to deliver via C-section, you may not need to take antibiotics, even if youve tested positive for strep B. You should take the strep B test even if youve scheduled a C-section just in case you go into labor early.
Other Ages And Groups
- GBS bacteria may come and go in peoples bodies without symptoms.
- On average, about 1 in 20 non-pregnant adults with serious GBS infections die.
- The rate of serious group B strep disease increases with age:
- There are 10 cases in every 100,000 non-pregnant adults each year.
- There are 25 cases in every 100,000 adults 65 years or older each year.
Don’t Miss: Can You Donate Plasma While Pregnant
Role Of The Immune Cells At The Maternal
The placenta and maternal decidua serves as a multi-layered barrier rich in immune cells that separates maternal and fetal tissues . The placental disc is composed of a chorionic villous tree that is immersed in maternal blood, where gas and nutrient exchange takes place. Hematogenous pathogens can invade the placenta and gain access to the fetal circulation through the placental chorionic villi. Alternatively, maternal vaginal pathogens can ascend into the uterus through the cervix where they may either encounter the maternal decidua and chorioamniotic membranes or the placenta disc, depending on placental location . It is unusual for the placenta to cover the cervix, a condition called placenta previa, so we will consider the most typical scenario where a vaginal pathogen would encounter the maternal decidua and subsequently, the chorioamniotic membranes on its path into the amniotic fluid. Thus, the immune cell rich decidua and chorioamniotic membranes comprise a unique immune environment that can contribute to pathogen clearance or facilitate invasion depending on pathogen virulence and host response.
Will I Be Tested For Group B Strep In Pregnancy
Testing for group B strep is not routinely offered to all pregnant women in the UK. Testing is usually only offered to women who had GBS in a previous pregnancy. It is sometimes found by chance when you have vaginal or rectal swabs or a urine test for other reasons.
Routine testing is a controversial issue in the UK, though it is widely available in most other high-income countries. The UK National Screening Committee does not recommend testing all pregnant women. This is because:
- Many women carry the bacteria and, in the majority of cases, their babies are born safely and without developing an infection.
- Screening women late in pregnancy cannot accurately predict which babies will develop GBS infection.
- No screening test is entirely accurate. For example, between 17% and 25% of women who have a positive swab at 3537 weeks of gestation will be GBS negative at delivery. And between 5% and 7% of women who are GBS negative at 3537 weeks of gestation will be GBS positive at delivery.
- Many of the babies who are severely affected from GBS infection are born prematurely, before the suggested time for screening.
- Giving antibiotics to all carriers of GBS would mean that a very large number of women would receive treatment they do not need. This could harmful mum and baby.
However, most high-income countries offer universal testing to pregnant women. A major research trial has recently been funded to establish what is the best approach for the UK.
Don’t Miss: Can Donating Plasma Affect Getting Pregnant
Gbs Hijacks Host Epithelial
Figure 3 GBS exploits epithelial-mesenchymal transition and vaginal epithelial exfoliation to permit ascending infection. During vaginal infection, GBS binds integrins on the epithelial surface and activates integrin signaling that results in the breakdown of adherens junctions. Displaced -catenin translocates to the nucleus, activating transcriptional changes of -catenin targets associated with EMT. Expression of these transcripts in vivo leads to vaginal epithelial exfoliation, which facilitates GBS ascension to the uterus and is associated with increased risk for microbial invasion of the amniotic cavity and preterm birth.
How Does A Baby Get Gbs
In pregnant women, GBS is found most frequently in the vagina and rectum. GBS is different than strep throat, which is Group A Streptococcus. GBS can live in a pregnant woman’s body and cause symptoms and an infection. GBS can also live in a pregnant woman’s body and not cause any symptoms and not pose any danger to her health. In this situation, the woman is called a “carrier.”
Early infection: Of the babies who become infected, most of the infections occur in the first week of life. In fact, most infection is apparent within a few hours after birth. , pneumonia, and meningitis are the most common problems. Premature babies face greater risk if they become infected, but most babies who get GBS are full-term.
Late infection: GBS infection might also occur in infants one week to several months after birth. Meningitis is more common with late-onset GBS-related infection than with early-onset infection. About half the babies who develop late-onset GBS got the infection passed to them from their mothers during birth. The source of the infection for others with late disease is thought to be contact with other people who are GBS carriers, or the GBS “carrier” mother after birth, or perhaps still other unknown sources. Late-onset infection is less common and is less likely to result in a baby’s death than early-onset infection.
Don’t Miss: Can You Get Lasik When Pregnant

