If You May Qualify For Medicaid Or The Childrens Health Insurance Program
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
Can A Pregnant Woman Receive Medicaid Or Chip Services Prior To An Eligibility Decision
Maybe. States may elect, but are not required, to provide some categories of Medicaid enrollees, including pregnant women, with presumptive eligibility. This allows pregnant women to receive immediate, same-day Medicaid services, typically at the clinic or hospital where they submit an application for Medicaid presumptive eligibility. Currently, 30 states provide presumptive eligibility to pregnant women.
Early Periodic Screening Diagnostic & Treatment
Early and Periodic Screening, Diagnostic, and Treatment benefit includes a comprehensive array of preventive, diagnostic, and treatment services for Medicaid eligible infants, children and adolescents under age 21, as specified in Section 1905 of the Social Security Act . The EPSDT benefit is also available to PeachCare for Kids® members up to 19 years of age. The EPSDT benefit is designed to assure that children receive early detection and care, so that health problems are averted or diagnosed and treated as early as possible. The goal of the EPSDT benefit is to assure that individual children get the health care they need when they need it.
The EPSDT benefit also covers medically necessary diagnostic services. When a screening examination indicates the need for further evaluation of a childs health, the child should be appropriately referred for diagnosis without delay. States are required to arrange for and cover under the EPSDT benefit any Medicaid covered service listed in Section 1905 of the Act if that treatment or service is determined to be medically necessary to correct or ameliorate defects and physical and mental illnesses or conditions for children through age 20 years of age.
Reviewing your Health Check Record
Billing Tips for Health Check
Health Check Referral Codes
Recommended Reading: Why Is Smoking Bad For Pregnancy
How Long Does The Eligibility And Enrollment Process Take
Texas Health and Human Services staff have 15 business days to process the application from the day they received it. Once eligibility is determined, the pregnant woman enrolls in a CHIP perinatal health plan on behalf of her unborn child. She has 15 calendar days to select a health plan from the day she gets a letter stating she can get CHIP perinatal benefits. If she does not choose a medical plan within the 15-day timeframe, HHS will choose one for her.
Read Also: Medicaid Office In Vicksburg Mississippi
If You May Qualify For Medicaid Or Childrens Health Insurance Program
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
Also Check: Can I Use Vagisil Wash While Pregnant
You May Like: How Early To Tell If Pregnant
Who Is Eligible For Medicaid In Georgia
As of April 2020, criteria for enrollment in Georgia Medicaid are set at the following levels for non-disabled adults:
- Children up to age 1 with family income up to 205% of federal poverty level
- Children ages 1-5 with family income up to 149% of FPL
- Children ages 6-18 with family income up to 133% of FPL
- Pregnant women with family income up to 220% of FPL
- Parents of minor children with family income up to 35% of FPL
Learn How To Apply For Medicaid In Texas
UPDATE: In 2020, most of the requirements for Medicaid are expected to remain the same.
Where do you sign up for Medicaid in Texas? You must first learn how to apply for Medicaid before you can start reaping the benefits of this federal- and state-sponsored medical assistance program that provides free or low-cost health insurance. You can proceed with your Medicaid application forms in Texas once you have confirmed your eligibility.
It is not a question of where to apply for Medicaid in Texas, but rather how you complete the process. When it comes to filing your application for Medicaid, there are several methods of which you can employ. However, the options for both how and where to apply for TX Medicaid vary in comparison to other states.
To learn some of the different ways you can submit a Texas Medicaid application, review the details provided in the sections below:
Also Check: Lice Treatments While Pregnant
Don’t Miss: How To Treat Headache During Pregnancy
Georgia Pregnancy Medicaid Income Limit
In addition to the income limit above, you have to also meet the following requirements:
What Does RSM Medicaid Cover?
Right from the Start Medicaid for pregnant women pays for medical care for pregnant women, including labor and delivery, for up to 60 days after they give birth. Benefits include:
Read Also: Medicaid How Much Money Can You Make
Texas Medicaid Application And Qualifications
It is easy to confuse Medicaid with Medicare. The two programs are not without their similarities. One key difference is that Medicare is a federal program, whereas Medicaid is a state program with rules that vary depending on where you are. The other major difference is that Medicare is based largely on age and disability, while Medicaid is based largely on income.
Depending on your circumstances, you can be on both at the same time. Circumstances is the key word. Medicare tends to be long-term, if not permanent. Medicaid is often a shorter-term solution. There are other programs that are generally associated with Medicaid such as financial and grocery assistance. It is possible that if you have qualified for these other forms of assistance, Medicaid will be included.
You May Like: How To Control Thyroid During Pregnancy
Who Is Eligible For Medicaid
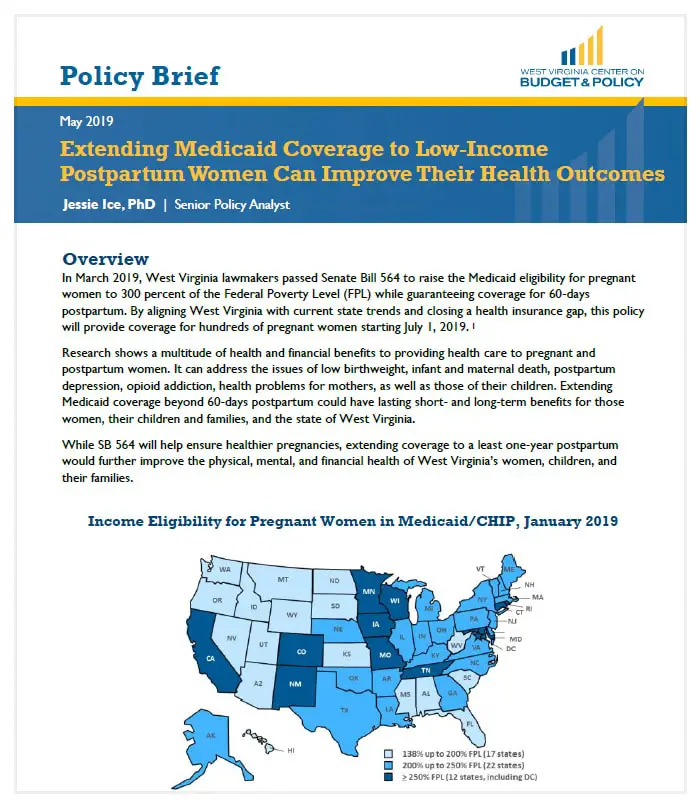
The general guidelines for eligibility for Medicaid are set by the Federal government however, each state sets up their own specific requirements for eligibility and these can differ from state to state.
All States are required to include certain individuals or groups of people in their Medicaid plan.
The state eligibility groups are:
- Categorically needy
- Medically needy
In the categorically needy group, this will cover pregnant women whose income level is at or below 133% of the Federal Poverty level.
In the medically needy group, this will cover a pregnant woman who makes too much money to qualify in the categorically needy group. This means that women, who may have been denied Medicaid before, may be able to qualify now.
Who Can Get Medicaid In Texas
You should apply for Medicaid if your income is low and you match one of the descriptions below:
- You think you are pregnant
- The parent or caretaker of a child and/or teenager under the age of 19.
- You are a child or teenager age 18 or under.
- An adult age 65 or older.
- You are legally blind.
- Living with a disability or disabled.
- You are in need of nursing home care.
Don’t Miss: How To Bounce Back After Pregnancy
Get Important News & Updates
Sign up for email and/or text notices of Medicaid and other FSSA news, reminders, and other important information. When registering your email, check the category on the drop-down list to receive notices of Medicaid updates check other areas of interest on the drop-down list to receive notices for other types of FSSA updates.
Effective Date Of Coverage
Once an individual is determined eligible for Medicaid, coverage is effective either on the date of application or the first day of the month of application. Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Also Check: How Can I Terminate Pregnancy
Even If Youre Not Sure Fill Out The Medicaid Application
The Centers for Medicare & Medicaid Services advises you to complete a Medicaid application even if youre not sure you qualify. Remember that its better for you to apply for Medicaid and be turned down than not to apply at all. A caseworker will review your case to determine whether or not you qualify for Medicaid benefits. Your Medicaid eligibility can change from year to year, so you may want to complete a new Medicaid application each year, even if your application was previously turned down.
Dont Miss: Is It Possible To Get Pregnant Without Ovulating
How To Fill Out The Get And Sign Free Proof Of Pregnancy Letter From Doctor Pdf Pdf Word Eforms Free On The Web:
By making use of SignNows comprehensive service, youre able to carry out any needed edits to Get And Sign Free Pregnancy confirmation letter PDF Word EForms Free , generate your customized digital signature in a couple of fast steps, and streamline your workflow without the need of leaving your browser.
Create this form in 5 minutes or less
Dont Miss: Can I Use Vagisil Wipes While Pregnant
Read Also: Can I Get Pregnant If I Have Irregular Periods
Apply For Medicaid For Children Only
Apply Online: You can apply online for this program at www.myflorida.com/accessflorida/.
Apply by mail or fax. You can apply for Medicaid for children through fax or email.
- You can email your application and documents to the address listed on this page
Children eligible for Medicaid can also receive benefits under Florida KidCare Program. In fact, Medicaid is a part of Florida KidCare program. Advantage of applying for Florida KidCare is that applications rejected due to higher income will be automatically transferred to Florida Healthy Kids.
You can find more information about this program HERE.
Dont Miss: Can Pregnancy Make Your Stomach Hurt
Missing Out On Billions In Federal Funding
By refusing Medicaid expansion under the ACA, Texas has already missed out on billions in federal funding that would otherwise have flowed to the state to provide medical care for their low-income residents. And in addition, the states emergency rooms are providing $5.5 billion in uncompensated care each year, treating patients who dont have health insurance. If Medicaid eligibility had been expanded, uncompensated care would have dropped considerably, so hospitals and business groups across the state have been pressuring lawmakers to relent on their opposition to Medicaid expansion.
Because Texas has refused to expand Medicaid, the federal government has warned the state that continued access to federal funding to help cover uncompensated care is in jeopardy . But Governor Greg Abbott has continued to reject Medicaid expansion, and described the federal governments tactics as coercive .
Since residents in states not expanding Medicaid still have to pay federal taxes, there has been a significant outflow from Texas residents to fund Medicaid expansion in other states. Over a decade , Texas residents will pay $36.2 billion in federal taxes that will be used to pay for Medicaid expansion in other states.
This is by far the highest of any state the next highest is Florida, where residents will pay just over $20 billion to pay for other states Medicaid expansion by 2022 .
Also Check: How To Workout When Pregnant
What Changes When A Woman Already Enrolled In Medicaid Becomes Pregnant
Generally, nothing. A woman who was previously eligible and enrolled in full-scope Medicaid who becomes pregnant continues to be eligible, and will be able to access pregnancy services. A woman who becomes pregnant while enrolled in Medicaid Expansion can stay in that coverage, at least until redetermination. The state must inform the woman of the benefits afforded to pregnant women under other coverage categories, such as pregnancy-related Medicaid, and provide the option to switch categories if the woman is eligible.
Preventing Maternal Deaths In Georgia
Comprehensive postpartum care is an important component to preventing maternal mortality. Georgia ranks no. 49 among states for the rate of maternal mortality, defined as deaths related to pregnancy that occurred during or within one year of the pregnancy or birth.
Georgia established a Maternal Mortality Review Committee in 2014 to identify maternal deaths and their causes. The committee found that between 2012 and 2014, 101 mothers died from pregnancy-related causes and about 60 percent of the deaths were preventable.
The committee also found significant evidence of the maternal mortality crisis Black women are facing in Georgia. The maternal mortality rates for Black women in Georgia were three to four times higher than for white women. The committee, as well as House Study Committee on Maternal Mortality and House Study Committee on Infant and Toddler Social and Emotional Health, included the postpartum Medicaid extension in their recommendations to help address the maternal mortality crisis.
Currently no states have implemented the postpartum Medicaid extension, but several states are pursuing the option through Medicaid 1115 waivers. Applying for a waiver is the only way to enact the policy and get federal Medicaid matching funds, unless proposed federal legislation passes to make it a state option.
Also Check: Can You Get Restylane While Pregnant
Colorado Indigent Care Program
The Colorado Indigent Care Program provides discounted health care services to low income people and families. CICP is not a health insurance program. Services vary by providers.
Who Qualifies?
You must be 18 and olderYou must be at or below 250% of the Federal Poverty Level You must be lawfully present in the United States and a legal resident of ColoradoYou cannot be eligible for Health First Colorado or Child Health Plan Plus
Top Benefits:
Discounted health care services provided by participating Colorado hospitals and clinicsNo premium costsYou are allowed to have primary health insurance or have MedicareCICP ratings are good for a full year, see program information page for exceptions
Co-pay Costs:
How To Apply For Medicaid
There are two ways to apply for Medicaid, the first of which is by speaking directly to your state Medicaid agency.
First, you need to find out what your states Medicaid policy is called as they tend to be named differently across America.
For example, in Hawaii the scheme is called Med Quest, while in Louisiana its called Healthy Louisianna.
You can find out what its called in your state using this free Government tool.
Youll then need to follow the individual plans application process.
The second option is to fill out an application through the governments Health Insurance Marketplace , providing details such as your income and how much dependants you have.
If youre eligible, your information will be sent to your state agency who will contact you about enrolling on the scheme.
If it turns out that youre not eligible, HIM will let you know if you qualify for a discounted individual insurance plan due to your circumstances instead.
Also Check: Do You Know If Your Pregnant First Week
Also Check: Can You Get Pregnant With Polycystic Ovaries
What Is The Cost
None. Medicaid law prohibits states from charging deductibles, copayments, or similar charges for services related to pregnancy or conditions that might complicate pregnancy, regardless of the Medicaid enrollment category. HHS presumes pregnancy related services includes all services otherwise covered under the state plan, unless the state has justified classification of a specific service as not pregnancy-related in its state plan. States may, however, impose monthly premiums on pregnant women with incomes above 150% of FPL and charge for non-preferred drugs.
Most states that cover pregnant women in their CHIP program do not have cost-sharing or any other fees associated with participation in the program.

