How Can I Prevent Gestational Diabetes
There are no guarantees when it comes to prevention, but the more healthy habits you can adopt before pregnancy, the better. If youve had gestational diabetes, these healthy choices may also reduce your risk of having it again in future pregnancies or developing type 2 diabetes in the future.
- Eat healthy foods Choose foods high in fiber and low in fat and calories. Focus on fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without compromising taste or nutrition. Watch portion sizes.
- Keep active exercising before and during pregnancy can help protect you from developing gestational diabetes. Aim for 30 minutes of moderate activity on most days of the week. Take a brisk daily walk. Ride your bike. Swim laps. Short bursts of activity such as parking further away from the store when you run errands or taking a short walk break all add up too.
- Start pregnancy at a healthy weight if youre planning to get pregnant, losing extra weight beforehand may help you have a healthier pregnancy. Focus on making lasting changes to your eating habits that can help you through pregnancy, such as eating more vegetables and fruits.
- Dont gain more weight than recommended gaining some weight during pregnancy is normal and healthy. But gaining too much weight too quickly can up your risk of gestational diabetes. Ask your doctor what a reasonable amount of weight gain is for you.
Signs Of Gestational Diabetes With Pregnancy
NursesPrime | 10/24/2021 | Signs of Gestational Diabetes with Pregnancy-Related Toxicity.
Signs of Gestational Diabetes with Pregnancy-Related Toxicity.
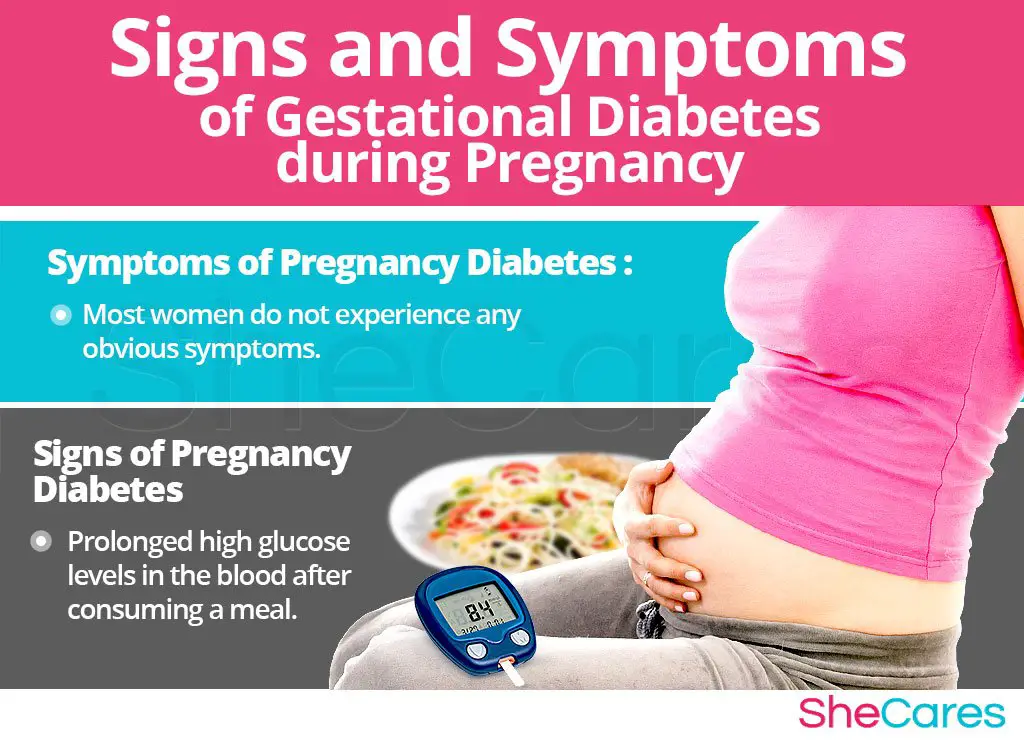
Gestational diabetes is diabetes that is first diagnosed during the second half of pregnancy, that is, after 24 weeks. Usually, suppose diabetes is identified in early pregnancy. In that case, it means the person was already living with type 2 diabetes and was just unaware of it.
Gestational diabetes generally develops during pregnancy and is reversed after a childs birth. Nonetheless, those diagnosed with gestational diabetes are at greater risk of developing type 2 diabetes later in life. CDC data indicates that each year 2 to 10% of pregnancies are affected by gestational diabetes.
What Are The Risks Factors Associated With Gestational Diabetes Mellitus
Although any woman can develop GDM during pregnancy, some of the factors that may increase the risk include the following:
-
Overweight or obesity
-
Family history of diabetes
-
Having given birth previously to an infant weighing greater than 9 pounds
-
Race
-
Prediabetes, also known as impaired glucose tolerance
Although increased glucose in the urine is often included in the list of risk factors, it is not believed to be a reliable indicator for GDM.
You May Like: Pregnancy Side Effects By Week
Who’s At Risk Of Gestational Diabetes
Any woman can develop gestational diabetes during pregnancy, but you’re at an increased risk if:
- your body mass index is above 30 use the BMI healthy weight calculator to work out your BMI
- you previously had a baby who weighed 4.5kg or more at birth
- you had gestational diabetes in a previous pregnancy
- 1 of your parents or siblings has diabetes
- you are of south Asian, Black, African-Caribbean or Middle Eastern origin
If any of these apply to you, you should be offered screening for gestational diabetes during your pregnancy.
What Are Clinical Trials And Are They Right For You
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
Read Also: Can You Get Lasik While Pregnant
How Is Gestational Diabetes Managed
If you are diagnosed with gestational diabetes, its important to follow your doctors advice. Managing the condition and keeping your blood glucose levels under control helps avoid complications for both you and your baby.
You may be referred to an obstetrician and dietitian and may need more frequent antenatal appointments and regular monitoring of your blood sugar levels.
What Is The Optimal Method Of Diagnosis
Since there is no clear glucose threshold above which pregnancy outcomes responsive to glycemic management occur , controversy persists as to the best diagnostic thresholds to define GDM. The International Association of the Diabetes and Pregnancy Study Groups Consensus Panel decided to create new diagnostic thresholds for GDM based on data from the Hyperglycemia and Adverse pregnancy Outcome study. IADPSG thresholds are the maternal glucose values from HAPO associated with a 1.75-fold increase of LGA, elevated C-peptide, high neonatal body fat or a combination of these factors, compared with the mean maternal BG values of women studied in HAPO. These arbitrary thresholds, when applied to the HAPO cohort, led to a GDM incidence of 17.8%. The National Institute of Health 2013 Consensus Conference summary statement stated that at present, the panel believes that there is not sufficient evidence to adopt a 1-step approach, such as that proposed by the IADPSG . However, since this publication, national organizations have published guidelines that are divergent in their approach to screening and diagnosis of GDM , thus perpetuating the international lack of consensus on the criteria for diagnosis of GDM.
Figure 1Preferred approach for the screening and diagnosis of gestational diabetes.
Figure 2Alternative approach for the screening and diagnosis of gestational diabetes.
Recommended Reading: Vagisil Safe While Pregnant
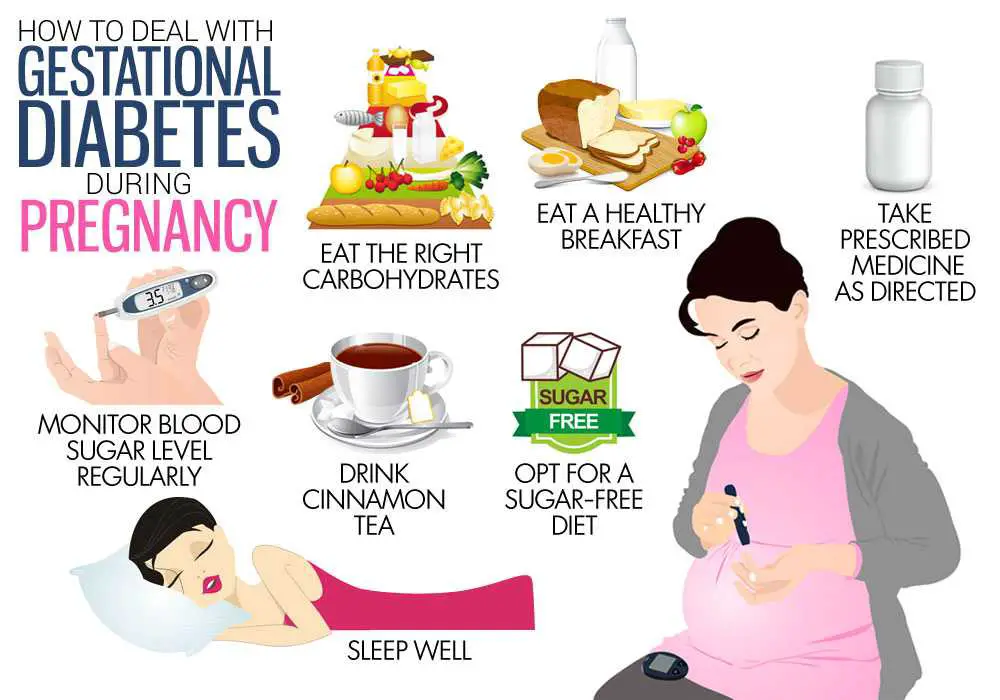
Is There A Special Diet Plan For Women With Diabetes During Pregnancy
While there is no one specific diet that is recommended for all women with gestational diabetes, following a meal plan can help keep your blood sugar levels under control and avoid complications.
- A nutritionist may be helpful in designing a meal plan that takes into account individual schedules and preferences.
- Eating a variety of foods is recommended, and it is better to eat smaller portions throughout the day rather than just a few large meals.
- Many women with gestational diabetes will be advised to eat fewer carbohydrates than in their normal diet and to eat complex carbohydrates that contain fiber. Its important to limit consumption of foods containing large amounts of simple sugars.
- High-fiber foods like fresh fruits and vegetables, as well as whole-grain products, are not only nutritious but also effective in keeping blood sugar levels stable.
- Skipping meals is not recommended because this leads to undesirable fluctuations in blood sugar levels.
How Does It Impact The Health Of The Mom And Baby
Gestational diabetes affects both mom and baby. The mom may experience weight gain and increased sugar levels. There may be hormonal fluctuations, too, which can cause mood swings. Pregnant women with gestational diabetes also have a higher rate of Cesarean sections. If the baby is larger, theres also a higher rate of shoulder dysplasia, which could be traumatic to the baby. In the long-term, the baby potentially has a higher risk of experiencing metabolic issues, earlier onset of diabetes, along with high blood pressure, thyroid abnormalities, and polycystic ovary syndrome. One thing leads to another, Dr. Yu explains.
Don’t Miss: Vagisil Cream Pregnancy
How Is Gestational Diabetes Mellitus Diagnosed
The American Diabetes Association recommends screening for undiagnosed type 2 diabetes at the first prenatal visit in women with diabetes risk factors. In pregnant women not known to have diabetes, GDM testing should be performed at 24 to 28 weeks of gestation.
In addition, women with diagnosed GDM should be screened for persistent diabetes 6 to 12 weeks postpartum. It is also recommended that women with a history of GDM undergo lifelong screening for the development of diabetes or prediabetes at least every three years.
Monitoring Your Blood Glucose Levels
Your medical team will give you a target range for your blood glucose levels. You will need to check these at home while you are pregnant.
You can purchase a blood glucose measuring kit from your local pharmacy or diabetes centre, or from Diabetes Australia in your state or territory call 1800 637 700 for help.
To test your blood glucose levels, you prick your finger with a lancet and put a small drop of blood onto a testing strip. Then you insert the strip into a meter, which reads your blood glucose level.
Also Check: Kinesio Tape For Pregnancy Round Ligament Pain
Early Signs Of Diabetes
Both types of diabetes have some of the same telltale warning signs.
- Hunger and fatigue. Your body converts the food you eat into glucose that your cells use for energy. But your cells need insulin to take in glucose. If your body doesn’t make enough or any insulin, or if your cells resist the insulin your body makes, the glucose can’t get into them and you have no energy. This can make you hungrier and more tired than usual.
- Peeing more often and being thirstier. The average person usually has to pee between four and seven times in 24 hours, but people with diabetes may go a lot more. Why? Normally, your body reabsorbs glucose as it passes through your kidneys. But when diabetes pushes your blood sugar up, your kidneys may not be able to bring it all back in. This causes the body to make more urine, and that takes fluids. The result: You’ll have to go more often. You might pee out more, too. Because you’re peeing so much, you can get very thirsty. When you drink more, you’ll also pee more.
- Dry mouth and itchy skin. Because your body is using fluids to make pee, there’s less moisture for other things. You could get dehydrated, and your mouth may feel dry. Dry skin can make you itchy.
- Blurred vision. Changing fluid levels in your body could make the lenses in your eyes swell up. They change shape and canââ¬â¢t focus.
What Happens If I Am Diagnosed With Gestational Diabetes

Like many other forms of diabetes,the best treatment is to control blood sugar levels through diet and possibleinsulin therapy. Your doctor will monitor your blood levels throughout your pregnancy,and you may also have to self-monitor your own blood glucose levels. Diet andexercise management helps with the condition, but insulin therapy may berequired.
When diagnosed early and treated,the risk of complications goes down dramatically. Women who are diagnosed and treatedeffectively go on to deliver healthy babies. Maintaining your health duringpregnancy is the best way to ensure you have a healthy birth. Regular prenatalcare and pregnancy care services also increase the chances of a healthypregnancy.
For more information on how toensure a healthy pregnancy, find out how Walnut Hill OBGYN Associates can helpyou with your pregnancy and prenatal care.
Also Check: Giving Plasma While Pregnant
Why Gestational Diabetes Occurs
It is not fully understood by science. Nonetheless, it is not difficult to guess that it is caused by widespread hormonal and metabolic changes in the body.
One of the reasons could be that the body needs a higher amount of most hormones, including insulin, during pregnancy. However, some women develop insulin resistance in reaction to these higher insulin levels.
Monogenic Diabetes In Pregnancy
Since pregnancy may be the first time in their lives that women undergo glucose screening, monogenic diabetes may be picked up for the first time in pregnancy. Monogenic diabetes first diagnosed in pregnancy should be suspected in the women with GDM who lack risk factors for GDM and type 1 diabetes and have no autoantibodies . A detailed family history can be very helpful in determining the likely type of monogenic diabetes. This is important because the type of monogenic diabetes influences fetal risks and management considerations. The most common forms of monogenic diabetes in Canada are maturity onset diabetes of the young 2 or MODY 3 . A history of family members with longstanding isolated elevated FBG with mild A1C elevations that do not progress to frank diabetes over a long duration is suggestive of MODY 2. During pregnancy, the usual phenotype for MODY 2 of isolated elevated FBG is not always seen, even though this phenotype may be present outside of pregnancy in the same woman . Fetal carriers of GCK mutations do not usually have macrosomia. Fetuses without the GCK mutation of mothers with GCK mutation are at increased risk of macrosomia. The best way to manage women with GCK mutation during pregnancy has yet to be established, but regular fetal growth assessment can aid in the establishment of appropriate glucose targets during pregnancy for women with documented or strongly suspected GCK mutations.
Also Check: Can You Use Vagisil During Pregnancy
How Can I Prepare For Pregnancy If I Have Diabetes
If you have diabetes, keeping your blood glucose as close to normal as possible before and during your pregnancy is important to stay healthy and have a healthy baby. Getting checkups before and during pregnancy, following your diabetes meal plan, being physically active as your health care team advises, and taking diabetes medicines if you need to will help you manage your diabetes. Stopping smoking and taking vitamins as your doctor advises also can help you and your baby stay healthy.
Prevention And Treatment Of Gestational Diabetes
Gestational diabetes can be scary, both for mother and baby. But the one positive thing about it is it is manageable.
There are multiple types of gestational diabetes. One can be managed through proper diet and exercise, and the other requires taking insulin and other medications.
Currently, diabetes has no cure. There are also no sure-fire ways to prevent getting gestational diabetes. What most professionals would advise, however, is to start practicing a healthy lifestyle. This would lower the chance of getting it. It also helps prevent you from getting it again if you had experienced it before in your previous pregnancy.
Here are some ways where you can start. You may also seek advice from your doctors to make sure any adjustments you will be making are appropriate for you.
Nix the sugary snacks. Cookies, candies, ice cream, and cake all sound delightful, but you wont be doing yourself any favors eating these. Instead, try to eat healthier.
Fruits can provide you with all the natural sugar you need. Add vegetables like carrots as well as whole grains to your diet. Just be careful and make sure you keep portions to what is acceptable.
- Get proper exercise and/or physical activity.
- Start your pregnancy at a healthy weight.
- Dont gain more weight than recommended.
- Check your blood sugar.
- Check your urine for ketones or chemicals that may indicate diabetes.
- More frequent doctor check-ups
Read Also: Can I Donate Plasma While Breastfeeding
Diabetic Eye Screening In Pregnancy
You will be offered regular diabetic eye screening during your pregnancy. This is to check for signs of diabetic eye disease .
Screening is very important when you are pregnant because the risk of serious eye problems is greater in pregnancy.
Diabetic retinopathy is treatable, especially if it is caught early.
If you decide not to have regular screening tests, you should tell the clinician looking after your diabetes care during pregnancy.
Read Diabetic eye screening.
Questions To Ask Your Doctor
- Im pregnant. Am I at risk for gestational diabetes?
- Is screening for gestational diabetes a standard part of my prenatal care?
- What tests do I need?
- Does gestational diabetes put my baby at risk for any health problems?
- Can I control gestational diabetes through lifestyle changes alone?
- What changes should I make to my diet and exercise?
- Will I need insulin? For how long?
- What follow-up tests or care will I need after I deliver my baby?
Recommended Reading: Donating Plasma While Trying To Conceive
Target Blood Glucose Levels During Pregnancy
Recommended daily target blood glucose numbers for most pregnant women with diabetes are
- Before meals, at bedtime, and overnight: 90 or less
- 1 hour after eating: 130 to 140 or less
- 2 hours after eating: 120 or less3
Ask your doctor what targets are right for you. If you have type 1 diabetes, your targets may be higher so you dont develop low blood glucose, also called hypoglycemia.
Checking Your Blood Sugar Level
You’ll be given a testing kit that you can use to check your blood sugar level.
This involves using a finger-pricking device and putting a drop of blood on a testing strip.
You’ll be advised:
- how to test your blood sugar level correctly
- when and how often to test your blood sugar most women with gestational diabetes are advised to test before breakfast and one hour after each meal
- what level you should be aiming for this will be a measurement given in millimoles of glucose per litre of blood
Diabetes UK has more information about monitoring your glucose levels.
You May Like: Vagisil And Pregnancy
Monitoring Blood Glucose Levels
Monitoring your blood glucose levels is essential. It gives you a guide as to whether the changes you have made to your lifestyle are effective or whether further treatment is required.
A diabetes nurse educator can teach you how and when to measure your blood glucose levels. They will discuss the recommended blood glucose levels to aim for.
Your doctor or diabetes educator can help you register with the National Diabetes Services Scheme for discounted blood glucose strips. Regular contact with your diabetes educator or doctor is recommended.
Management: Healthy Behaviour Interventions
Weight gain. The 2009 IOM guidelines for weight gain during pregnancy were developed for a healthy population and little is known regarding optimal weight gain in women with GDM. Retrospective cohort studies of GDM pregnancies show that only 31.7% to 42% had GWG within IOM guidelines. Those gaining more than the IOM recommendations had an increased risk of preeclampsia , caesarean deliveries , macrosomia , LGA and GDM requiring pharmacological agents . Modification of IOM criteria, including more restrictive targets of weight gain, did not improve perinatal outcomes of interest . A large population-based study including women with GDM, concluded that while pre-pregnancy BMI, GDM and excessive GWG are all associated with LGA, preventing excessive GWG has the greatest potential of reducing LGA risk . These researchers suggest that, in contrast to obesity and GDM prevention, preventing excessive GWG may be a more viable option as women are closely followed in pregnancy.
Further studies are needed to develop weight gain guidelines for GDM patients and to determine whether weight gain less than the IOM guidelines or weight loss in pregnancy is safe. Until this data are available, women with GDM should be encouraged to gain weight as per the IOM guidelines for the BMI category to reduce adverse maternal and neonatal outcomes and postpartum weight retention.
Don’t Miss: Vagisil Wipes During Pregnancy

