What Are The Most Probable Etiologies Of Her Thrombocytopenia
Causes of thrombocytopenia may be specific complications of pregnancy or have no relationship to pregnancy per se, although some of them may occur with increased frequency during gestation . Incidental thrombocytopenia of pregnancy, usually referred to as gestational thrombocytopenia, accounts for 70%-80% of cases. It occurs in the mid-second to third trimester, and its pathogenesis is unclear. It has been speculated that it may result from various mechanisms, including hemodilution and accelerated clearance. No confirmatory laboratory tests are available, and the diagnosis is one of exclusion. Thrombocytopenia is typically mild to moderate, with approximately two-thirds of cases having platelet counts 130-150 × 109/L. The literature is not consistent in where a cut-off in platelet count is concerning however, we consider a platelet count < 80 × 109/L as a trigger to conduct further investigations for an alternative etiology. We consider a diagnosis of gestational thrombocytopenia unlikely if the platelet count is < 50 × 109/L, with very few cases having been described with counts 40-50 × 109/L., For the thrombocytopenia to be consistent with gestational thrombocytopenia, women should have no past history of thrombocytopenia , the thrombocytopenia resolved spontaneously within 1-2 months after delivery, and the fetus/newborn baby should not have had thrombocytopenia .
What Does It Mean When You Have A Low Platelet Count In Pregnancy
If your skin is wounded or broken, platelets clump and form coagulation to prevent bleeding. You cant develop clots when you dont have sufficient platelets in your blood.
Thrombocytopeniamay also be called a low platelet count. Depending on the underlying cause,this disease can vary from mild to severe.
For some, thesymptoms may include severe bleeding and, if not handled, may be deadly. Theremay be no symptoms for other individuals.
Studies Of Itp In Pregnancy
Cook et al reviewed a 10-year experience with treatment of ITP, which included 25 women and 32 infants. Platelet counts were obtained in 23 of 32 newborns. Of 8 infants with low platelets at birth, 3 were mild, 3 were moderate, and 2 were severe. A total of 6 infants had severe thrombocytopenia at birth or during the neonatal period. Median platelet nadir occurred 4 days following delivery. Eighteen cesarean deliveries were performed, 6 with complications .
The authors reviewed the literature over 20 years, which included 474 women with ITP. Approximately 15% of infants were found to have severe thrombocytopenia . The incidence of intracranial hemorrhage among infants with severe thrombocytopenia was 4% after cesarean delivery, compared with 5% after vaginal delivery
Burrows and Kelton reported on a large series of maternal platelet counts collected on all women admitted to labor and delivery over a 6-year period at McMaster University , as well as cord blood platelet counts at the time of delivery . Of 46 women with ITP, 4 infants were born with severe thrombocytopenia. Three of these 4 infants were delivered vaginally, and 1 was delivered by cesarean delivery. No infant experienced an intracranial hemorrhage.
Their literature review of 18 studies on maternal ITP involved 601 neonates. Severe thrombocytopenia occurred in 72 of 601 neonates . Intracranial hemorrhage occurred in 6 out of 601 neonates and was unrelated to mode of delivery. PUBS complication rate was 4.6%.
Don’t Miss: Does Short Term Disability Cover Pregnancy
How Can Having Low Platelets Affect My Pregnancy And Birth Plan
In February, a very pregnant Mandy Moore, star of the popular TV series “This Is Us,” revealed that she had to alter her birth plan due to a diagnosis of low blood platelets. Though Moore didn’t elaborate on what specifically changed, low platelets is a fairly common condition.
Platelets, also called thrombocytes, are the smallest human blood cells and play a crucial role in blood clotting. Released by your bone marrow, the quantity of these specialized cells in your blood is generally reported on a complete blood count .
Pregnancy is generally a pro-clotting state, which makes sense clotting helps protect women from excessive bleeding at delivery. But there is a delicate balance between activities that help your blood clot and those that cause too much clotting.
At their best, platelets combine with other factors in the blood that control bleeding and help plug holes in the walls of blood vessels.
At their worst, platelets can form clots in the blood vessels in areas that have plaque buildup. This can put you at increased risk for heart attacks and strokes. When you have too few platelets, called thrombocytopenia, maternal complications such as excessive bleeding, premature delivery, or inability to get an epidural can arise.
Diagnosis And Differential Diagnosis
Pregnancy-related versus nonpregnancy-related
Causes of thrombocytopenia may be specific complications of pregnancy, be associated with an increased frequency in pregnancy, or have no relationship to pregnancy.
Pregnancy-specific complications
Gestational thrombocytopenia, also known as incidental thrombocytopenia of pregnancy, is the commonest cause of thrombocytopenia in pregnancy occurring in approximately 75% of cases. It is a diagnosis of exclusion, no confirmatory tests are available. It generally causes mild thrombocytopenia with the majority of cases having platelet counts of 130 to 150 x 109/L. Most experts consider this diagnosis unlikely if the platelet count falls below 70 x 109/L.
It occurs in the middle of the second trimester and the third trimester and is not associated with maternal bleeding. During pregnancy, it is not possible to differentiate between the more severe form of gestational thrombocytopenia and primary immune thrombocytopenia as both are diagnoses of exclusion. For the thrombocytopenia to be consistent with gestational thrombocytopenia, women should have no history of thrombocytopenia , the thrombocytopenia should resolve spontaneously within 1 to 2 months in all cases and the fetus/neonate should not be affected by thrombocytopenia.
Pregnancy-associated conditions
Nonpregnancy associated
Viral infection
Diagnostic approach
ITP
> 30 x 109/L â no treatment required in 1st and 2nd trimesters
> 50 x 109/L â procedures safe
Treatment
TTP/HUS
Don’t Miss: Why Am I So Bloated I Look Pregnant
Causes Of Low Mpv Levels
The following conditions have been known to result in abnormally low levels of MPV:
Inflammatory bowel disease : Average platelet size decreases due to Crohns disease and ulcerative colitis. Treatment for IBD will help increase MPV.
Rheumatoid arthritis: Low MPV levels have been reported in patients with active rheumatoid arthritis, but levels tend to also increase after treatment.
Viral infections: A respiratory viral infection is diagnosed through low mean platelet volume readings in a CBC. Respiratory syncytial virus infection patients also often show a low MPV.
Appendicitis: Low MPV can help determine an acute appendicitis diagnosis. When stomachaches are due to appendicitis, there will likely be low MPV. MPV in the CBC is needed to diagnose appendicitis accurately.
Autoimmune disorders: Low MPV levels are often common in a number of autoimmune disorders. For instance, low mean platelet volume has been observed in active lupus cases, rather than in people without a flare-up.
Certain cancers: Bone marrow cancer can cause a low mean platelet volume. Research shows that low MPV with platelet distribution width will help treat and diagnose bone marrow metastasis.
Familial Mediterranean fever : This is an autosomal recessive hereditary disease where there are frequent attacks of fever, arthritis, pleuritis, peritonitis, or erysipelas-like skin disease. Lower MPV is expected in FMF patients when there is secondary thrombocytosis.
Low Platelet Count In Pregnancy Is Not Very Common
This is not a full exclusive list to detail causes of low platelet count in pregnancy but covers some of the common ones. Read essentials about normal platelet count in pregnancy.
Low platelet count in pregnancy is not a very common condition but can be present in a significant number of patients. It is found to be observed in nearly 5 to 8 percent of women in their pregnancy. The condition can be detected at an early stage with routine blood tests and follow up during the course of pregnancy. Therefore, regular check-up is essential.
The importance of regular follow-up cannot be emphasized enough.
Ctrl+D
- READ MORE
You May Like: What Tylenol Is Safe For Pregnancy
What Can The Patient Expect During A Subsequent Pregnancy
A review of the clinical courses of 92 women with ITP during 119 pregnancies over an 11-year period found women with previously diagnosed ITP were less likely to require therapy for ITP than those with newly diagnosed ITP, although the frequency of bleeding complications did not differ between the 2 groups. Platelet counts at delivery were < 150 × 109/L in 89% of women. In most cases, thrombocytopenia was mild to moderate and the pregnancies were uneventful however, 31% required intervention to increase the platelet count at some time during their pregnancy. Thrombocytopenia was observed in 31 of 109 of infants 11 had platelet counts lower than 50 × 109/L. Two fetal deaths were recorded, one of which was caused by hemorrhage.
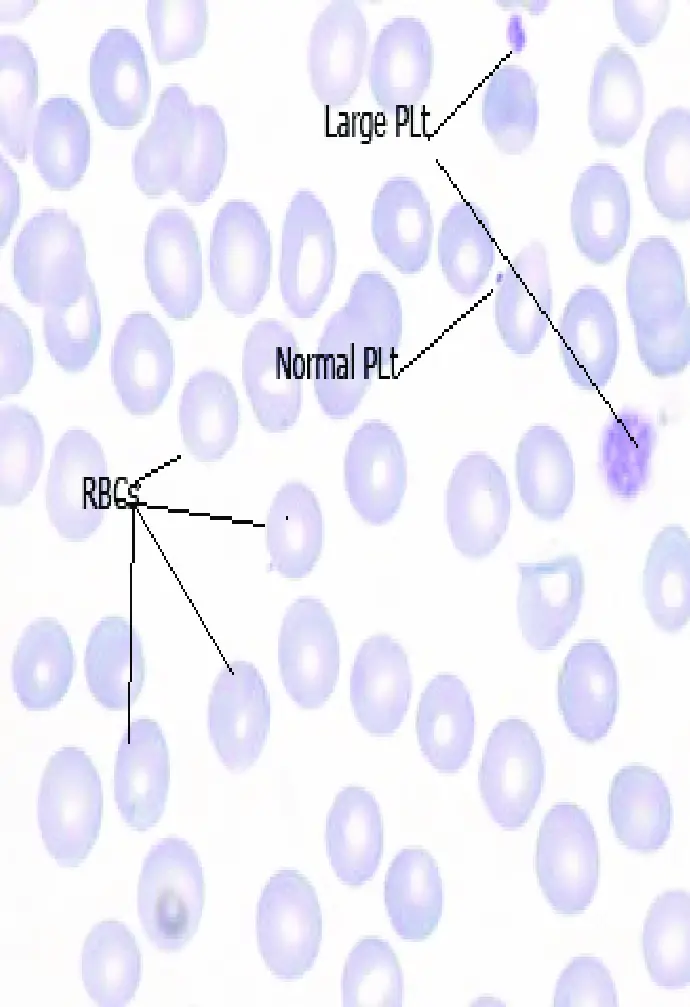
Normal And Abnormal Platelet Counts
A complete blood count test is a standard panel of bloodwork. The platelet count is one of things this test measures. Here is what various platelet counts mean:
- Normal: Between 150,000 and 450,000 platelets per microliter of blood
- Low: Below 150,000 platelets per microliter
- Mild bleeding risk: Below 50,000 platelets per microliter
- Serious bleeding risk: 10,000 to 20,000 platelets per microliter or lower.
You May Like: What To Eat At 7 Weeks Pregnant
How Often Should The Patient Be Monitored And What Will Be The Indication For Treatment Of Thrombocytopenia
The frequency of platelet counts in pregnant women with thrombocytopenia should be based on clinical reasoning because no evidence is available. When we have a high level of confidence that a patient has gestational thrombocytopenia, we check the platelet count at the time of each routine prenatal visit. Women should also have the blood count repeated 1-3 months after delivery to assess whether spontaneous resolution of the thrombocytopenia has occurred.
If the diagnosis is ITP or uncertain, we check the platelet count every 2-4 weeks, depending on the stability of the platelet counts. If platelet counts are found to be < 80 × 109/L after week 34, we monitor them on a weekly basis.
The presence of gestational thrombocytopenia does not generally alter the management of pregnancy. However, in a few patients, the low platelet count may compromise the ability to deliver epidural anesthesia and general anesthesia represents a greater risk. For women with platelet counts of 50-80 × 109/L, in whom a diagnosis of ITP cannot be excluded, we give 10 mg of prednisone once daily starting 10 days before the anticipated date of delivery. Others may start with a higher dose and adjust downward, but there are no published randomized trials to guide management. Alternatively, some experts also advise a course of intravenous immunoglobulin , 1 g/kg in 1 or 2 divided doses, which may be useful both diagnostically and therapeutically.
Low Blood Platelets In Pregnancy
The reason for low platelets in pregnancy is because the body produces more of plasma during this period, which means there is more fluid and less platelets in each milliliter of blood. However, this does not cause any problem to the mother or child. In case the platelet count is less than what it should be the doctor will ask for the blood test to be redone. A low platelet count could result in bleeding during or even after the birth and doctors have to be cautious about this.
Certain health conditions are the cause of low platelet counts and could be there before the pregnancy too. Lupus is one such problem of the immune system blood thinners like heparin affect the platelet count and certain types of cancer. A low platelet count could also be a sign of pre-eclampsia. Symptoms for his syndrome are headaches, pain above the abdomen, protein in the urine and high blood pressure.
You May Like: How To Lose Weight Quickly After Pregnancy
What Does It Mean To Have Gestational Thrombocytopenia
Platelets are blood cells that aid in clotting. Doctors measure platelets by the count per microliter of blood.
- Normal platelet count:150,000-400,000/microliter.
- Mild thrombocytopenia: 100,000-150,000/microliter.
Pregnant women tend to have higher rates of mild thrombocytopenia, but researchers arent really sure why that is. We know that a low platelet count results from the bodys tendency to use up or destroy platelets faster than it can produce them. It appears that pregnancy speeds up the bloods natural renewal processes, but its not clear why this happens.
Some pregnant women already have a non-pregnancy-related type of thrombocytopenia, called immune thrombocytopenic purpura . Symptoms are bruising and purple spots on the skin, caused by spontaneous bleeding.
Some medicines, such as the blood-thinning drug heparin, can also affect your platelet count. Maternal platelet count and antiplatelet antibodies do not predict the risk of neonatal thrombocytopenia. In some cases, the low platelet count may compromise the ability to deliver epidural anesthesia and general anesthesia represents a greater risk. Mothers platelet levels will go back to a normal range 12 months after the delivery.
The good news is that typically, cases of gestational thrombocytopenia will disappear after delivery.
How Can We Explain Her Clinical Deterioration And Worsening Thrombocytopenia
The HELLP syndrome affects 10%-20% of women with severe preeclampsia, but 15%-20% of patients do not have antecedent hypertension or proteinuria. Criteria for the diagnosis of HELLP syndrome have been published by Sibai and include hemolysis , aspartate aminotransferase > 70 U/L, and a platelet count < 100 × 109/L. The Martin et al criteria are less stringent and include an LDH > 600 U/L, an aspartate aminotransferase > 70 U/L and a platelet count < 150 × 109/L. A partial form of the disease among women with severe preeclampsia has been described, in which only 1 or 2 of the 3 components of the syndrome are present. Approximately 70% of women with HELLP have evidence of the syndrome antepartum and 30% develop it postpartum.
You May Like: What To Expect When 10 Weeks Pregnant
What Is The Risk To The Neonate How Should He Be Monitored
Platelet counts < 50 × 109/L occur in 10% of newborns of mothers with ITP, whereas platelet counts < 20 × 109/L occur in 5% of cases. Intracranial hemorrhage has been reported in 0%-1.5%.,, There are no indirect ways of measuring the fetal platelet count, and the correlation between maternal and fetal platelet counts is poor., The best predictor of severe thrombocytopenia at birth is its occurrence in an older sibling,,, Maternal response to treatment does not automatically protect the newborn from the development of thrombocytopenia. On the other hand, there is no robust evidence to suggest that neonates from women with ITP poorly responsive or refractory to treatment have a higher risk of severe thrombocytopenia.
What Does Low Blood Platelets Count Mean
When you receive your blood test results and platelets count comes low in CBC test, that means:You dont have enough platelets in your blood which makes your body to be unable to form clots properly, you will have a tendency of bleeding upon injury more than the healthy person,Mild low platelets count is less significant and means transient state, pre-recovery, or variation of laboratories.However, in severe platelets deficiency you may show superficial bleeding in the skin that appears as a rash of tiny-sized purple spots , usually seen on the lower legs and forearms as well as excessive bruising Low Blood Platelet count doesnt necessarily mean you have a cancer, more blood tests for cancerso that please carefully read the possible reasons to understand your platelets level then you have the right to ask about your results.
purpura looks like on hand foot skin
Don’t Miss: What Are My Chances Of Getting Pregnant At 41
What Every Clinician Should Know
Thrombocytopenia, defined as a platelet count less than 150 x 109/L, is second only to anemia as the most common hematologic abnormality encountered during pregnancy,occurring in 7% to 10% of pregnancies. Platelet counts less than 100 x109/L are observed in only 1% of pregnant women, which is the definition adopted by an International Working Group published in Blood in 2010.
In normal pregnancy, platelet count is approximately 10% lower than in the nonpregnant state and decreases as gestation progresses. Despite this, most women will still have platelets within the normal level. In the majority of cases of thrombocytopenia in pregnancy, the thrombocytopenia is mild and not associated with significant morbidity for the mother or the fetus or neonate.
Occasionally, thrombocytopenia may be part of a serious medical disorder with significant morbidity for mother and fetus, and the challenge facing clinicians is to determine the level of risk it poses to the mother and fetus.
Symptoms Of Low Platelets
A low platelet count can cause a variety of symptoms. Call your doctor if you notice these issues or if they become more frequent or severe:
- Easy bruising, also called purpura
- Petechiae, tiny red spots on your skin
- Excess bleeding after even minor injuries
- Pain in your joints, particularly large joints like the knees and hips
- Frequent nosebleeds
- Vaginal bleeding after menopause or unusually heavy vaginal bleeding
You May Like: Does Medical Abortion Affect Future Pregnancy
What Is The Evidence For Specific Management And Treatment Recommendations
Burrows, R, Kelton, JG. âFetal thrombocytopenia and its relation to maternal thrombocytopeniaâ. N Engl J Med . vol. 329. 1993. pp. 1463-6.
Jensen, JD, Wiemeier, SE, Henry, E, Silver, RM, Christensen, RD. âLinking maternal platelet counts with neonatal platelet counts and outcomes using data repositories of a multihospital health care systemâ. Am J Perinatalol. vol. 28. 2011. pp. 97-604.
Gernsheimer, TB. âThrombocytopenia in pregnancy: is this immune thrombocytopenia orâ¦â. Hematology Am Soc Hematol Educ Program. vol. 2012. 2012. pp. 198-202.
Myers, B. âDiagnosis and management of maternal thrombocytopenia in pregnancyâ. Br J Haematol. vol. 158. 2012. pp. 3-15.
Provan, D, Stasi, R, Newland, AC, Blanchette, VS, Bolton-Maggs, P. âInternational consensus report on the investigation and management of primary immune thrombocytopeniaâ. Blood . vol. 115. 2010. pp. 168-86.
No sponsor or advertiser has participated in, approved or paid for the content provided by Decision Support in Medicine LLC. The Licensed Content is the property of and copyrighted by DSM.

