Do I Automatically Qualify For Medicaid If Im Pregnant
If you are pregnant and have a low income or no income, you may want to apply for Medicaid as soon as possible. Medicaid covers prenatal health care throughout the pregnancy, labor, and delivery, and for an additional 60 days postpartum. Your child automatically qualifies if she or he is born while youre on Medicaid.
Recommended Reading: I Have Medicaid And Im Pregnant
How Can I Get Financial Assistance While Pregnant
Dont Miss: Apply For Medicaid When Pregnant
If You May Qualify For Medicaid Or Childrens Health Insurance Program
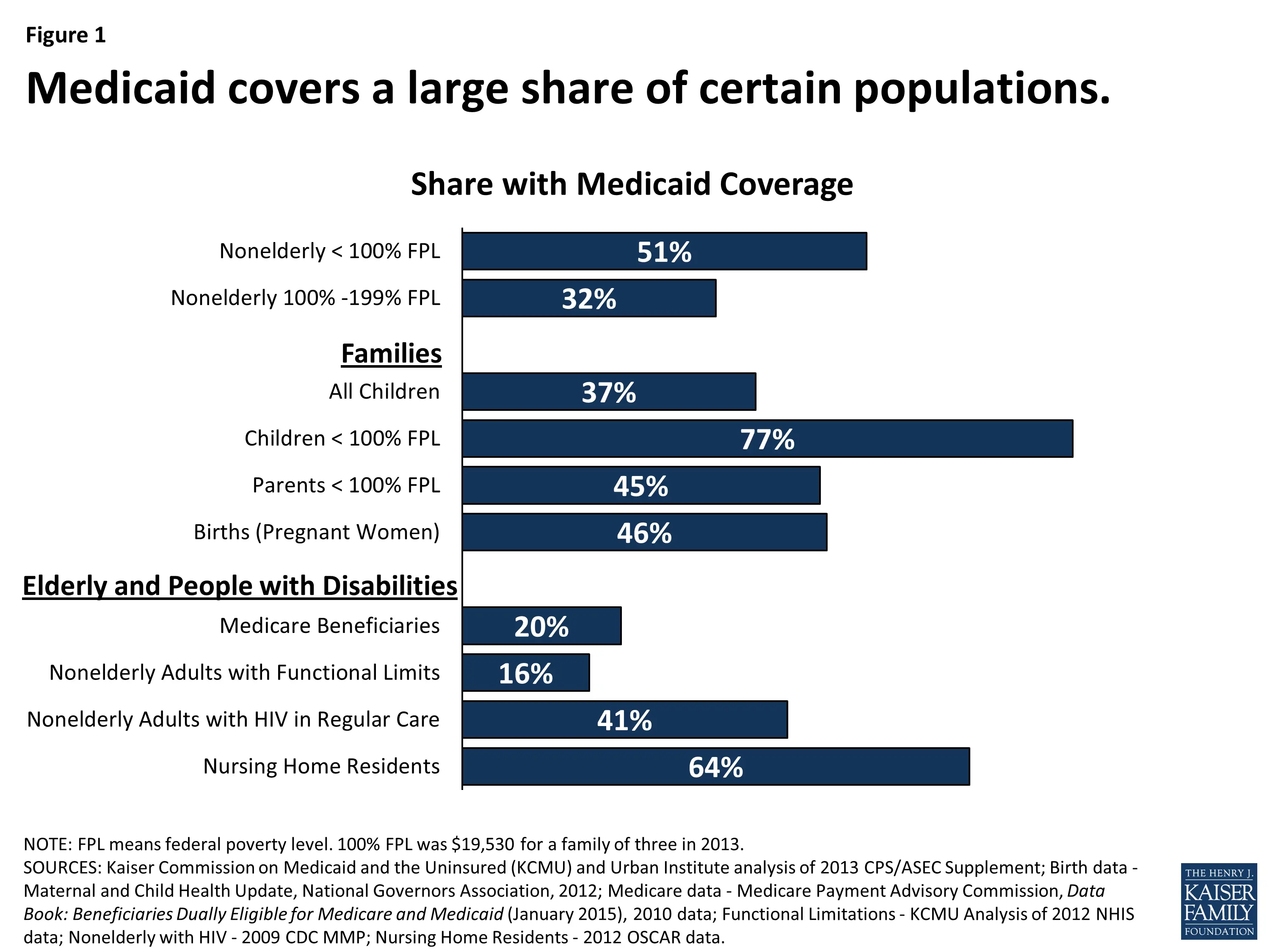
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
Also Check: Is Beth On Good Girls Pregnant
Medicaid For Pregnant Women Eligibility
Pregnant women will be able to enjoy benefits through presumptive eligibility. Presumptive Eligibility for Pregnant Women provides Medicaid to pregnant women in emergency who may need instant parental care. Women with income less than 185% of federal poverty level can qualify to receive Medicaid through PEPW.
Simplified Eligibility for Pregnant Women is another way to get qualified for full Medicaid cover. Pregnant women qualifying for PEPW can then apply for SEPW and get full coverage which would not be available with PEPW.
Emergency Medical Assistance For Non

- Individual must have Medical Assistance basis of eligibility
- Individual must have a genuine medical emergency
- Individual must be a resident of Florida
Medical emergency purposes for EMA can include:
- Chronic medical condition which can place individualâs health in dangerous condition if left unattended
- Chronic medical condition which can cause impairment to the body if left unattended
- Chronic medical condition which can cause some body organs to dysfunction if left unattended
- Individual has a sudden onset of conditions that can result in acute symptoms
Donât Miss: How To Cancel Medicaid In Virginia
Recommended Reading: Can You Sue If You Get Pregnant On Iud
Lawsuit Over Arkansas Medicaid Work Requirement Was Slated For Scotus But Hearing Was Canceled And Work Requirement Waiver Was Then Rescinded By Hhs
The Trump administration appealed the case, as expected, and a panel of three judges on the U.S. Court of Appeals for DC heard oral arguments in the appeal in October 2019. During the arguments, all three judges expressed concerns about the coverage losses that stem from Medicaid work requirements, which was the crux of Boasbergs ruling earlier in the year that suspended the work requirement. And in February 2020, the three-judge panel unanimously ruled that it was arbitrary and capricious for HHS to approve the Arkansas Works waiver, and upheld Boasbergs ruling to overturn the states Medicaid work requirement. So the work requirement has remained suspended.
In July 2020, however, the Trump administration asked the Supreme Court to intervene and allow Arkansas to reinstate its work requirement once the COVID-19 situation is under control enough to allow the unemployment rate to return to normal levels. The Supreme Court justices agreed to hear the case, and oral arguments in the lawsuit, Arkansas v. Gresham, were scheduled for March 29, 2021 at the Supreme Court.
But the Biden administration does not support Medicaid work requirements, and asked the Supreme Court to cancel the hearing. That request was granted, and Arkansas v. Gresham was not heard by the Supreme Court.
Dont Miss: Lasik During Pregnancy
Programs For Pregnant Women
Snapshots are informational only. You must apply to find out what programs or waivers you qualify for.
If you are not looking to find coverage for pregnant women, please choose another category.
You May Like: Can I Be Pregnant At 48 Years Old
What If Im Turned Down By Medicaid
- You may be able to buy a private health plan through the Marketplace instead for the 2018 plan year in the fall. You may qualify for savings based on your income through a premium tax credit and savings on out-of-pocket costs.
- If you dont qualify for either Marketplace or Medicaid savings, you still have options. Learn more here.
Can You Switch Insurance During Pregnancy
Switching insurance during pregnancy is possible.
You can switch insurance plans any time during the open enrollment, or at any point if you have a qualifying life event, regardless of whether or not you are pregnant, says Dodge.
He also mentions that pregnant women may want to consider switching to a health insurance plan with a lower deductible or higher coverage for hospitalization if theyre able to switch plans before giving birth. This will help lower your out-of-pocket costs.
Also Check: Anthem Blue Cross Medicaid Nevada
You May Like: Is Laser Lipo Safe During Pregnancy
Is A Woman Who Has Access To A Family Members Employer
Possibly. If the employer-sponsored insurance is unaffordable or not MEC, the woman is eligible for APTCs. Affordability is determined by the IRS standards for the percentage of income a person is expected to spend on insurance. This calculation applies to the cost of the employees insurance, not the cost of the family plan. That means that if the premiums for the employees insurance are affordable, no member of the family is eligible for an APTC. If the individuals premium is unaffordable, the family will be eligible for APTCs in an amount determined by their income and the premium cost.
Get Important News & Updates
Sign up for email and/or text notices of Medicaid and other FSSA news, reminders, and other important information. When registering your email, check the category on the drop-down list to receive notices of Medicaid updates check other areas of interest on the drop-down list to receive notices for other types of FSSA updates.
Read Also: Can I Get Pregnant With Ms
Reduced Coverage / Medicare Cost Sharing Or Premium Payment
Qualified Medicare BeneficiariesCovered group: individuals covered by MedicareIncome limits: Income cannot exceed 100% of the federal poverty level. For more information, view the Guidelines for Medicare Cost-Sharing Programs brochure.Age: Medicare beneficiaries of any ageQualifications: Individuals must be eligible for Medicare Part A hospital insurance.
Medicaid In New York State

- COVID-19 News and Updates:
- COVID Information for Medicaid Consumers:
- Medicaid Coverage through Your Local Department of Social Services during the Coronavirus Emergency
- Medicaid Telehealth Services During the Coronavirus Emergency
- IRS Form 1095-B Update:
- The 1095-B form for Tax Year 2020 is no longer being mailed automatically.If you need a copy of your 1095-B for Tax Year 2020, you can request it:
Also Check: How To Know Know If You Are Pregnant
What Is Pregnancy Medicaid
Medicaid is a government-sponsored health insurance program for low-income families who have no medical insurance or inadequate insurance. All states offer Medicaid or a program similar to Medicaid to help pregnant women receive adequate prenatal and postpartum care. Medicaid also offers health insurance to seniors, children, and people with disabilities.
Lawfully Residing Targeted Low
States have the option to provide CHIP and Medicaid coverage to children and pregnant women who are lawfully residing in the United States and are otherwise eligible for coverage, including those within their first five years of having certain legal status. If states do not adopt this option, federal law requires a 5-year waiting period before many legal immigrants are permitted to enroll in Medicaid and CHIP. Learn more about providing health coverage to lawfully residing children and pregnant women at 2107 of the Social Security Act, and in SHO# 10-006. A list of states providing Medicaid and CHIP coverage to lawfully residing children and/or pregnant women.
Don’t Miss: What Pregnancy Test Gives The Earliest Results
What Changes When A Woman Already Enrolled In Medicaid Becomes Pregnant
Generally, nothing. A woman who was previously eligible and enrolled in full-scope Medicaid who becomes pregnant continues to be eligible, and will be able to access pregnancy services. A woman who becomes pregnant while enrolled in Medicaid Expansion can stay in that coverage, at least until redetermination. The state must inform the woman of the benefits afforded to pregnant women under other coverage categories, such as pregnancy-related Medicaid, and provide the option to switch categories if the woman is eligible.
Maternity Coverage Is Still Way Too Complicated
Bethany married her college sweetheart a year and a half ago. But because her husband has had a few different jobs since graduating, most of which were contract positions with lackluster benefits, Bethany opted to stay on her moms insurance. Young adults can remain on their parents insurance until theyre 26, regardless of marital status.
It seemed ideal: Her parents have had some health issues in recent years, which meant they always hit their deductible. They had no idea about the dependent exemptions until it was too late, Bethany says.
In hindsight, it would be more affordable if Bethany was unmarried and therefore had a lower household income so she could claim Medicaid benefits, or if she taken out her own policy through a marketplace. While there are some federal laws that protect maternity rights, Bethany falls into a loophole.
For years, federal laws have stipulated that employers need to cover maternity care for their employees and their spouses. But there are no laws that specifically state companies have to cover maternity care for adult children because, until the ACA passed in 2009, most employer-based health insurance plans cut off coverage when the children legally became adults or upon college graduation.
There are all these disparate puzzle pieces fitting together and not fitting together.Julie StichThe International Foundation of Employee Benefit Plans
Read Also: How To Know If Your Pregnant In Your Tubes
How Can I Apply For Lamoms
You must fill out an application form. If needed, someone can assist you in completing the form. You can get an application form from the Medicaid office in the parish where you live, at any of the participating Medicaid Application Centers, from our Web site by clicking here, or by calling 1.888.342.6207. The application form with your information can be mailed to your local Medicaid office.
How To Apply For Medicaid In Arkansas
The Arkansas Medicaid application process is an opportunity for residents who cannot afford health insurance to obtain medical coverage. Learning how to apply for Medicaid in AR is beneficial for families who meet the eligibility requirements to receive Medicaid benefits. It is important for prospective applicants to understand what will be on the AR Medicaid application form and where to apply for Medicaid insurance in the state. If you are wondering, Can you apply for Medicaid online? or Where do you sign up for Medicaid in Arkansas? continue reading the outlined information below.
Where do you sign up for Medicaid in Arkansas?
While many states allow applicants to apply for Medicaid online, the state of Arkansas does not have a way to sign up for Medicaid via web. However, you may print the Medicaid form from the internet and fax it to 870-534-3421 or mail the form to:
DHS Jefferson County
P.O. Box 5670
Pine Bluff, AR 71611
If you are enrolled in the program, workers at the county office will provide you with more information on what health care services Medicaid covers and which medical providers are available to you. They will also ask you to pick a primary care physician.
Find out more about the requirements to receive benefits from Medicaid in our free guide.
Information Required on the Medicaid Application Form in Alabama
- Your name, birth date and Social Security Number
- Your before-tax income
You May Like: Is Vagisil Safe To Use While Pregnant
Read Also: What Are The Odds Of Getting Pregnant With An Iud
Where To Apply For Medicaid In Arkansas In Person
If you need help filling out your Medicaid application form you can apply for Arkansas Medicaid in person. Many people who do not know how to apply for Medicaid choose this option to enlist the help of office employees. You can pick up, complete, and submit an application at the Department of Human Services office in the county where you live.
Furthermore, applicants can obtain more information about Medicaid regulations and program details. If you cannot make it in person, you can have a family member or friend apply for you. When you visit the Department of Human Services office, you should be ready with the information you need to apply for Medicaid.
As with the other methods of applying for Medicaid, applicants need all current insurance forms, pay stubs, verifiable identification and other necessary documents. If you do not have all of this information available, the state can still process your Medicaid application, but it may take longer to get the health insurance for which you are entitled.
After submitting an application, applicants waiting to hear about the case status may wait for a status update via mail or phone call. There will be further instructions available, based on each applicants unique case.
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your .
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
Dont Miss: How To Use Nutraburst
Recommended Reading: What Can I Eat Or Drink To Get Pregnant Fast
Help For Adults And Seniors To Stay Safely In Their Homes
DHS has several programs that are designed to help adults with physical disabilities and seniors stay in their homes and communities rather than go to s skilled nursing facility. To apply for the programs below, please reach out to your local county office. If you would like to talk to a counselor about your options, call the Choices in Living Resource Center at 1-866-801-3435 or email .
ARChoices in Home Care provides attendant care, home-delivered meals, personal emergency response systems, adult day services, and respite care. Independent Choices is like ARChoices in Home Care, but the client is responsible for hiring, training, and supervising his or her in-home workers from Medicaid funds the client or his/her representative control.
Living Choices Assisted Living is a Medicaid program that pays for apartment-style housing for people who need extra care and supervision. Its for people who are at risk of being placed in a nursing home or who are in a nursing home and want more independence.
Program of All-Inclusive Care for the Elderly is for people age 55 and older who have been determined by the state, based on specific criteria, to need nursing home care. PACE allows them to live as independently as they can.
Medicaid For Pregnant Individuals
When you are enrolled in Medicaid for pregnant members, you get comprehensive health care benefits during your pregnancy and for one full year following your babys birth. Medicaid may provide up to 3 months coverage prior to the date you apply. You also receive dental benefits during your pregnancy and postpartum. Dental services are administered through the Smiles For Children program.
Please visit CoverVA or CubreVirginia for more information on Medicaid for Pregnant Individuals.
Please contact the Smiles for Children program at 1-888-912-3456 for more information on dental services for pregnant members.
Navigate
Read Also: What Is Good For Constipation During Pregnancy
Medicaid For Pregnant Women & Chip Perinatal
Pregnant women might be able to get free health coverage during their pregnancy through Medicaid for Pregnant Women or the CHIP Perinatal program.
Medicaid provides health coverage to low-income pregnant women during pregnancy and up to two months after the birth of the baby.
CHIP Perinatal provides similar coverage for women who can’t get Medicaid and don’t have health insurance.
To get Medicaid for Pregnant Women or CHIP Perinatal, you must be a Texas resident. You must be a U.S. citizen or qualified non-citizen to get Medicaid for Pregnant Women.
If you have other health insurance, you are not eligible for the CHIP Perinatal program.
When you apply, we’ll ask about your family’s monthly income to see if you can get Medicaid or CHIP Perinatal.
Do Medicaid And Chip Provide Pregnant Women With Comprehensive Health Coverage
Yes, in most but not all states. Full-scope Medicaid in every state provides comprehensive coverage, including prenatal care, labor and delivery, and any other medically necessary services.
Pregnancy-related Medicaid covers services necessary for the health of a pregnant woman and fetus, or that have become necessary as a result of the woman having been pregnant. Federal guidance from the Department of Health and Human Services clarified that the scope of covered services must be comprehensive because the womans health is intertwined with the fetus health, so it is difficult to determine which services are pregnancy-related. Federal statute requires coverage of prenatal care, delivery, postpartum care, and family planning, as well as services for conditions that may threaten carrying the fetus to full term or the fetus safe delivery. The state ultimately decides what broad set of services are covered. Forty-seven states provide pregnancy-related Medicaid that meets minimum essential coverage and thus is considered comprehensive. Pregnancy-related Medicaid in Arkansas, Idaho, and South Dakota does not meet MEC and is not comprehensive.
CHIP coverage for pregnant woman is also typically comprehensive. However, in states where services are being provided to the pregnant woman by covering the fetus, the services may not be comprehensive with respect to the health needs of the pregnant woman.
Don’t Miss: How Could You Get Pregnant On Birth Control

